BACKGROUND: Pyeloplasty is commonly performed in the pediatric population for ureteropelvic junction obstruction. Literature on patient and surgical factors associated with perioperative complications has been limited to single institution studies and mainly focused on long term outcomes. We aim to determine the patient and surgical factors that contribute to 30 days morbidity after pediatric pyeloplasty using a national database. METHODS: This retrospective cohort study used the National Surgical Quality Improvement Pediatrics database to evaluate the patient and clinical factors associated with 30 days post- surgical outcomes in pediatric patients who had undergone open and laparoscopic pyeloplasty between 2012-2021. Patient factors evaluated included age, sex, race, history of prematurity (HOP), weight, and ASA classification. Surgical factors included operative time, preop creatinine, albumin, hematocrit, WBC, and prior steroid use. Complications were categorized using the Clavien-Dindo (CD) classification. 30 days readmission rate and most frequent complications were analyzed. Multivariate logistic regressions were performed to examine associations.
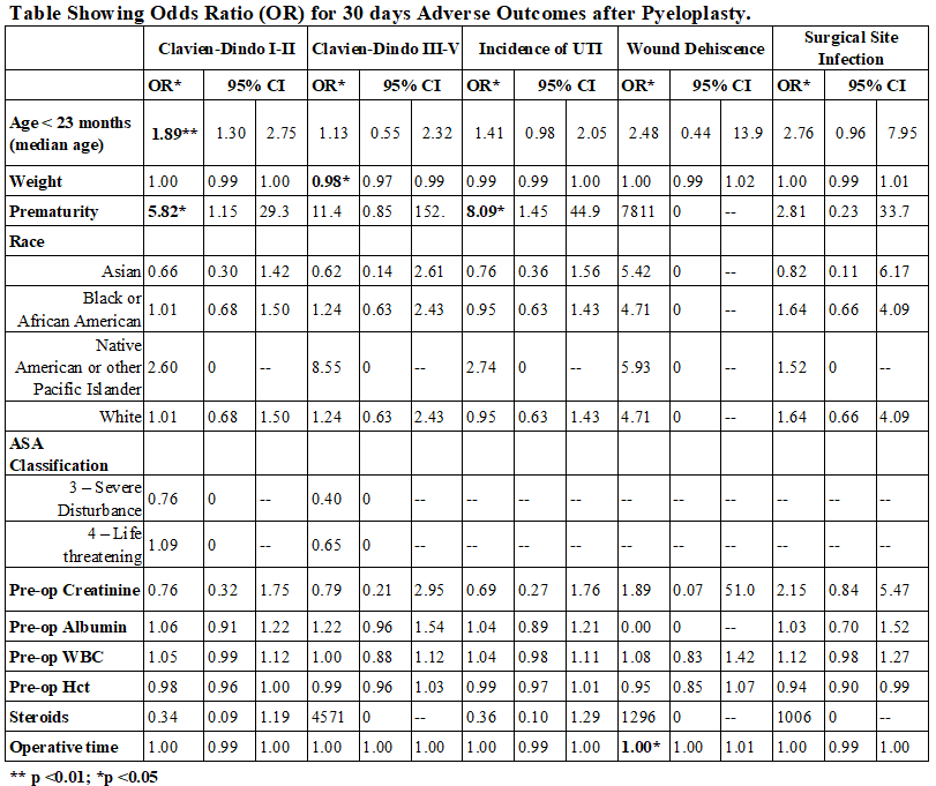
RESULTS: We identified 10,182 children who underwent pyeloplasty between 2012-2021. Cases with missing demographic data were excluded. 8,221 patients met inclusion criteria. There were 528 (6.4%) readmissions within 30 days. 30 cases, 0.4% were related to obstruction. UTI was the most frequent post-operative complication (n = 232, 2.8%). Median age at the time of surgery was 23 months, 90 patients were < 30 days old at the time of surgery. Age < 23 months and HOP were associated with CD I-II (OR 1.89, p <0.01 and 5.82, p <0.05 respectively). Low weight at time of surgery was associated with CD III-V (OR 0.98, p <0.05). HOP was also associated with incidence of UTI (OR 8.09, p <0.05). Prior steroid use in 35 patients was not associated with wound dehiscence or infection. There was a modest correlation between operative time and wound dehiscence (OR 1.006, p <0.05).
CONCLUSIONS: Complications after pyeloplasty are rare and most commonly due to UTI. HOP and low weight at the time of surgery were associated with increased complications after pyeloplasty. Prior steroid use was not associated with wound dehiscence or surgical site infection.