BACKGROUND: Suicide has risen to the eleventh leading cause of death in the United States with rates four times higher in men than women. Nearly half of individuals who commit suicide were seen by a non-behavioral health provider within four weeks of taking their life. Healthcare providers report a deficiency in training to assess patients regarding suicidal ideation (SI). The outpatient urology setting presents an opportunity to reduce suicide through screening male patients, offering behavioral health (BH) referrals, and providing staff education. Here we report on a standardized quality improvement suicide risk screening program for men presenting to an outpatient urology clinic.
METHODS: Male patients aged 18 and over presenting during a three-week pilot (Oct 2023) at a community urology office were offered depression and suicide screening using the validated Patient Health Questionnaire 9 (PHQ-9). Men who scored 10 or greater and/or indicated any ‘thoughts you would be better off dead or of hurting yourself’ (Question 9) were offered BH referral. Patients with positive Question 9 screening additionally received the Columbia Suicide Severity Rating Scale (C-SSRS). Data collected included PHQ-9 responses, age, race/ethnicity, BH diagnoses, reasons for urology visit, and positive screening outcomes. Office staff were offered suicide risk training consisting of in-person training, supporting documents, and a narrated presentation. Anonymous pre/post training assessments of staff knowledge and confidence were performed using selected questions from the validated Zero Suicide Workforce Survey. Statistical analyses were completed with Fisher’s exact and Wilcoxon Ranked Sum tests.
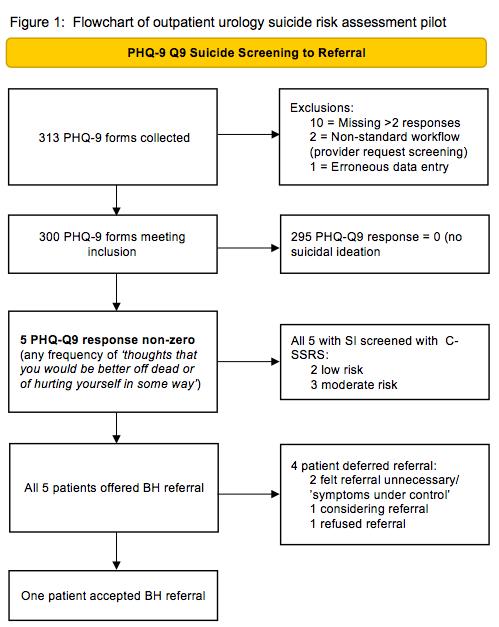
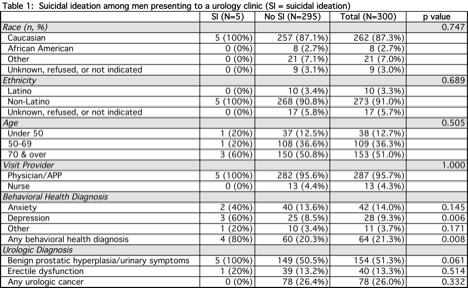
RESULTS: During the pilot, 313 of 497 (63%) men presenting to the clinic and meeting inclusion criteria were screened using the PHQ-9. After exclusions, data from 300 individuals were available for analysis (Figure 1). Five patients (1.7%) screened positive for suicide risk on Question 9 of the PHQ-9. Based on the C-SRSS, two were deemed low and three moderate risk. A pre-existing diagnosis of depression was more common among men with SI (60%) versus those without (8.5%) (Table 1). All five patients expressing SI were offered BH referrals with one accepting; the other four declined for various reasons but contracted for safety. Of the 22 office staff trained on SI assessment, 16 (73%) and 9 (41%) replied to the pre- and post-assessment, respectively. Post-assessment indicated better knowledge/comfort on all eight questionnaire items.
CONCLUSIONS: Suicide risk screening can be successfully implemented in an outpatient urology setting. In a pilot, 1.7% of men indicated SI at the time of urologic evaluation. While a minority of SI patients accepted a BH referral, all were assessed and provided with suicide safety information, representing an intervention they may have otherwise not received.