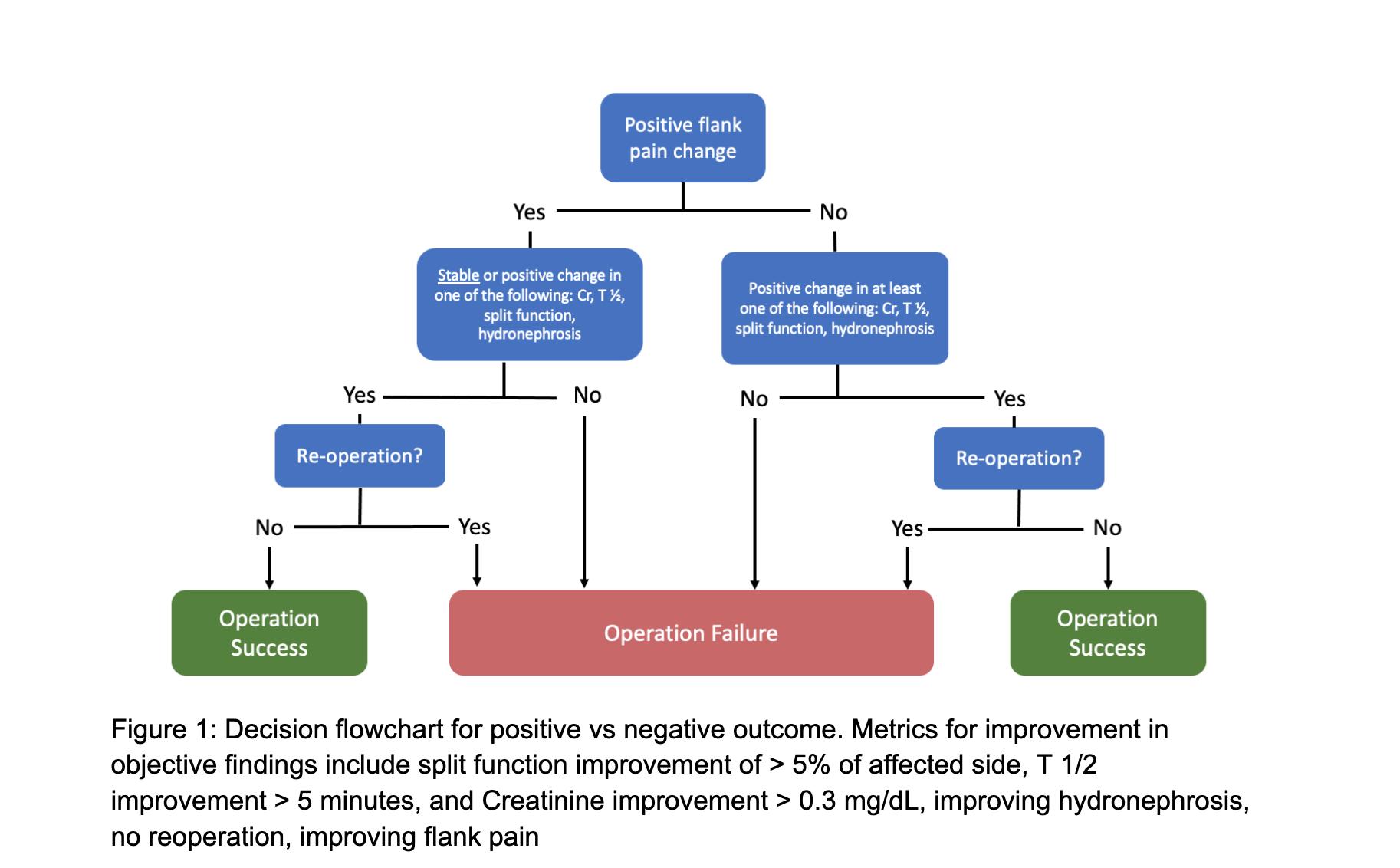
BACKGROUND: Patients with ureteropelvic junction obstruction (UPJO) often undergo pyeloplasty to address a reduction of kidney function or bothersome symptoms. However, guidelines and literature lack clear definitions of operative success. Here we evaluate the key factors of composite pyeloplasty success in a group of 216 patients treated at a multi-institution hospital system from 2015-2023. These factors include improvement in flank pain, split function change, improved T½ on a nuclear scan, stable or reduced hydronephrosis, avoidance of reoperation, and creatinine improvement. We aim to identify the components that strongly indicate overall pyeloplasty success to guide more focused future postoperative assessments.METHODS: Composite success variable was defined according to Figure 1. Patients were stratified by outcome and univariate analysis was performed using T-test and chi-square tests to identify significant differences. We then analyzed the ability of individual positive outcomes to predict overall composite success by comparing weighted F1 scores. F1 scores are the harmonic mean of precision and recall, and weighting accounts for the uneven distribution of outcomes.RESULTS: Of 216 adults aged 18-85 who underwent pyeloplasty for treatment of UPJO, 176 (81.5%) adults were considered to have a positive composite outcome based on the decision flowchart. Of the variables assessed, all individual outcomes were significantly associated with success (p≤0.02) except T½. Improving flank pain (F1=0.81), hydronephrosis (F1=0.78), and no re-operation (F1=0.81) were the most predictive of success.CONCLUSIONS: These results suggest that when patients present with flank pain and hydronephrosis, improvement of these findings may be the most appropriate measure of operative success in patients who did not undergo reoperation. These data also suggest that information derived from renal scans has limited predictive power of operative success 3-6 months post-surgery and may be deferred in straightforward cases to minimize unnecessary imaging. Future efforts would be directed towards increasing our study population and increasing demographic diversity to further assess our definition of success; in addition, a prospective trial looking at the utility of renal scans in a postoperative setting may be beneficial.