BACKGROUND:
The continuous effects of pelvic radiotherapy (RT) on urethral and surrounding tissue extend over several years (Stone et al., Lancet Onc. 2003). In the case of stress urinary incontinence (SUI), there is a delicate balance between avoiding artificial urinary sphincter (AUS) implantation during active inflammatory processes and delaying quality of life improvements for patients. Our study seeks to explore the optimal timing for placing an AUS post-RT.
METHODS:
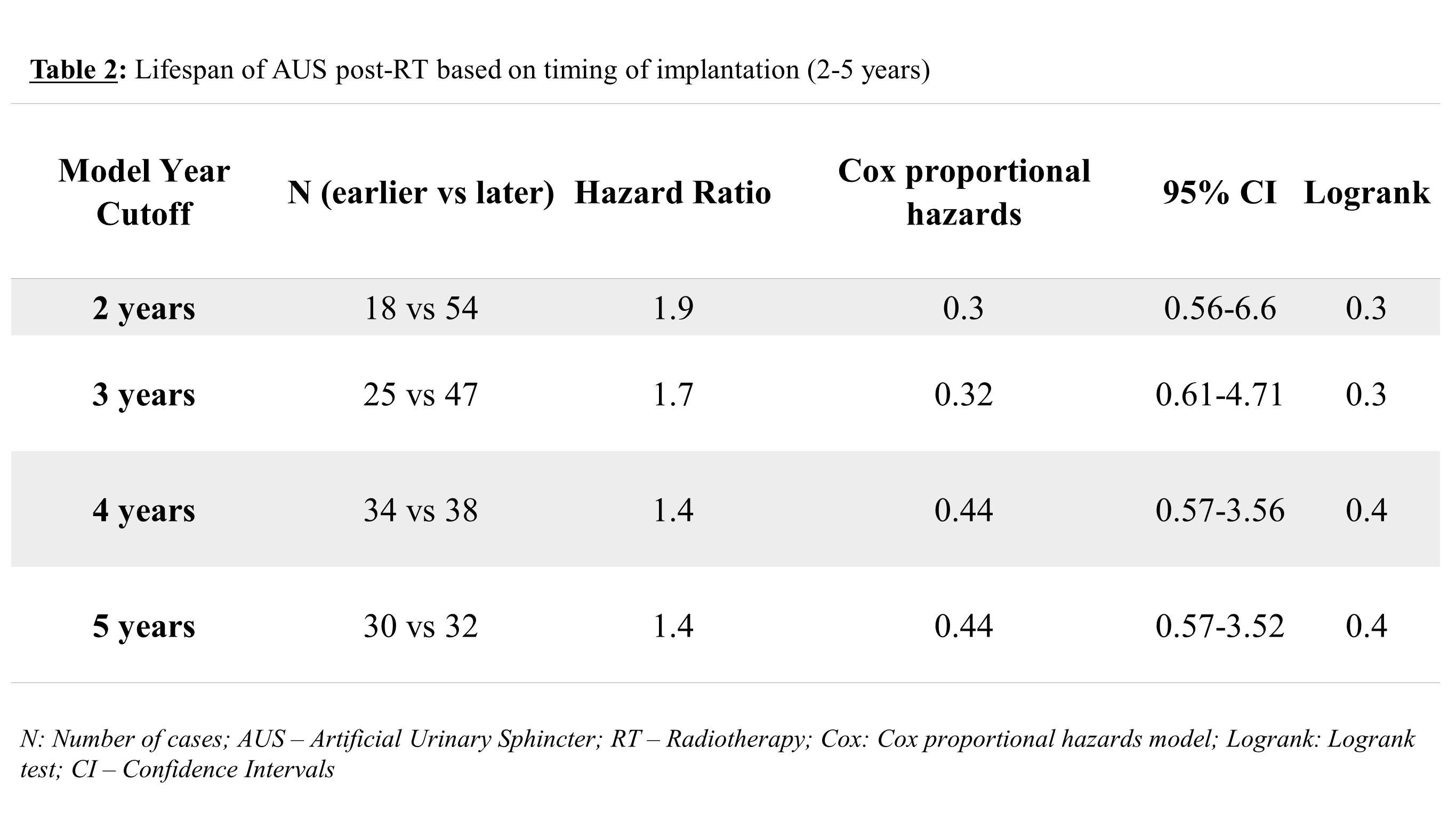
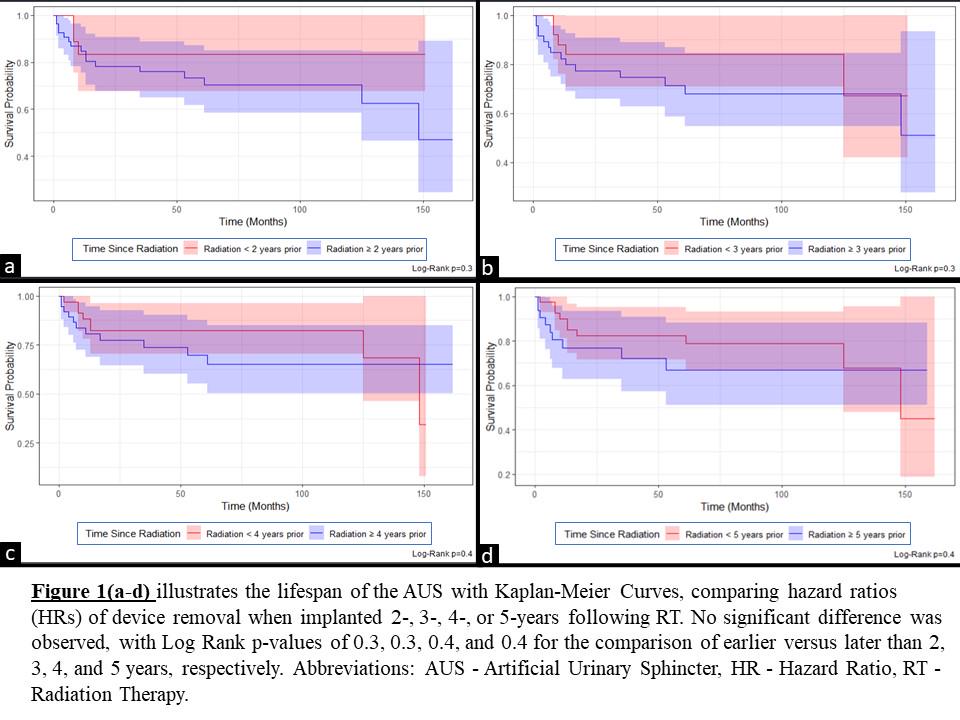
A retrospective review was conducted on initial AUS placements from two high-volume centers between January 1st, 2011, and July 1st, 2023. We included patients who had undergone their first (virgin) AUS placement after pelvic RT, whether RT was administered alone or as part of a combined approach with radical prostatectomy (RP). Exclusions comprised patients who underwent RT after AUS insertion in addition to those with incomplete key data. Variables collected included clinical demographics, procedure details, device outcomes, and indications for revisions/explantations (Rev/Exp). To determine the optimal timeline for device implantation post-RT, we compared hazard ratios (HRs) of device Rev/Exp within the years 2-5 following RT using Kaplan-Meier curves for each year (earlier vs. later than 2/3/4/5 years following RT). Statistical significance was determined by a log rank p.v. of 0.05. Data analysis was conducted using R 4.3 (R Core Team, 2023).
RESULTS:
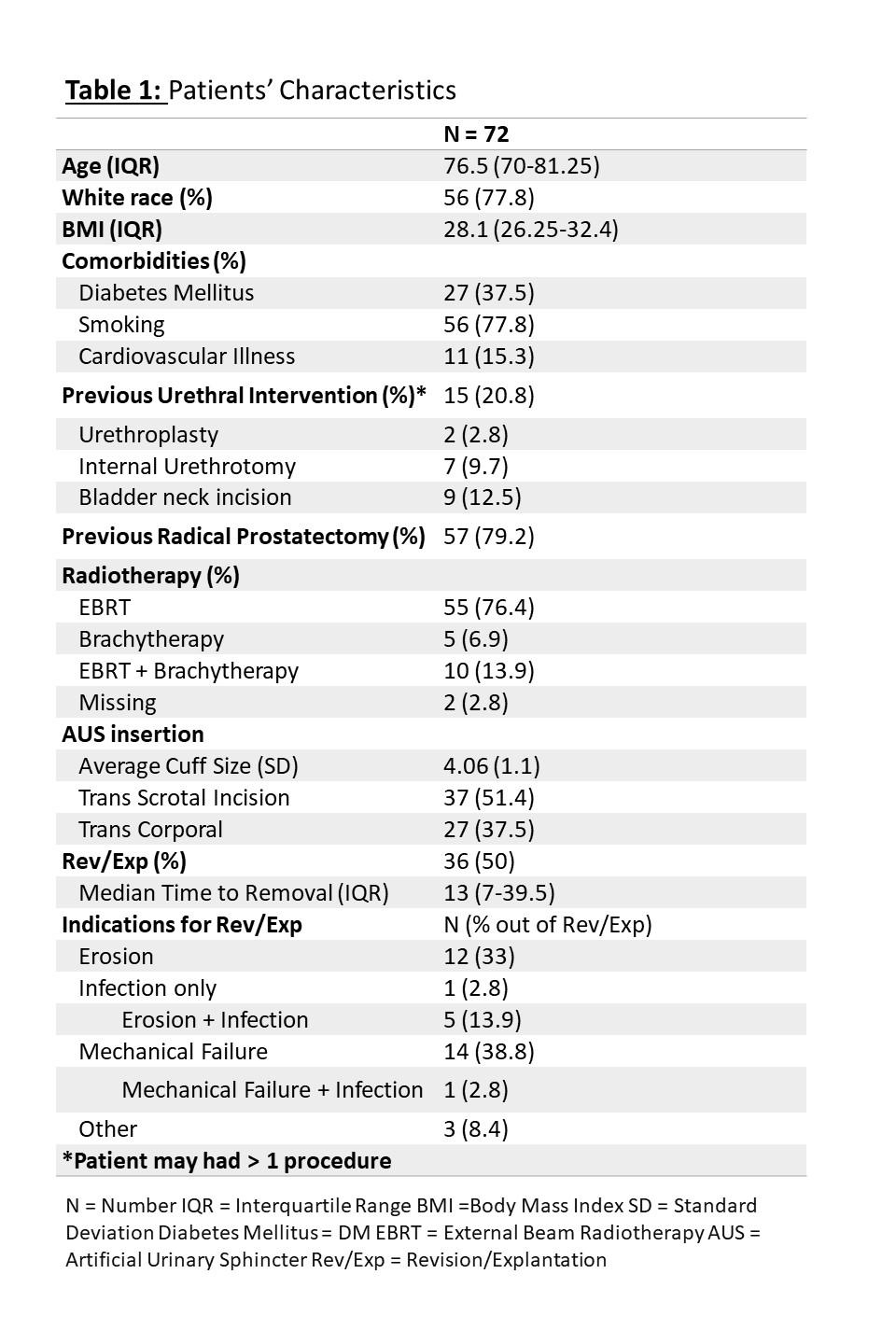
Overall, 72 patients met our inclusion criteria with a median age of 76.5 (IQR = 70 - 81.25), of whom 56 (77.8%) were white. 57 (79.2%) patients had undergone previous RP, and 15 (20.1%) had undergone one or more previous urethral/bladder neck interventions (urethroplasty 2[2.9%], Internal urethrotomy 7 [9.7%], and bladder neck incision [BNI] in 9 [12.5%]). Table 1 further details patients' comorbidities and AUS insertion parameters. After a median follow-up of 57.5 (13-107), a total of 36 (50%) devices were Rev /Exp, with mechanical failure (MF) in 14 (19.4%) followed by device erosion in 12 (16.7%) being the main reasons (Table 1). When implanted earlier versus later than 2-, 3-, 4-, or 5-years post-RT, Kaplan-Meier curves revealed no significant difference in the risk of device Rev/Exp. The p.values were 0.3, 0.3, 0.4, and 0.4, respectively, (Figure 1; Table2).
CONCLUSIONS:
The study findings suggest that implanting an AUS for SUI following RT within a 5-year timeframe results in comparable device lifespan and complication rates. However, the conclusions drawn from this high volume bi-institutional study with long follow-up may be limited by the small sample size. Currently, guidance for approach selection primarily depends on patient selection and surgeon preference based on the available data.