BACKGROUND: Hyperbaric Oxygen (HBO2) Therapy is used to treat radiation cystitis (RC), however, there is a lack of objective, non-invasive ways to measure its efficacy. The purpose of this pilot study is to explore feasibility of collecting and measuring preliminary concentrations of urine inflammatory biomarkers pre and post-HBO2 treatment for RC compared to controls.
METHODS: Following Institutional Review Board approval, adult patients with a diagnosis of severe Radiation Therapy Oncology Group (RTOG) grade 3 or higher diagnosed via cystoscopy were recruited. Mid-stream morning urine samples negative for bacterial infection were collected within one week of starting HBO2, and one week following HBO2. HBO2 was administered at a pressure of 240-250 kPa for 80-90 minutes, up to five times per week. Healthy controls were additionally recruited, and urine samples collected at two time points corresponding to average HBO2 time course. Urine biomarker data including Interleukin-6 (IL-6), Tumor Necrosis Factor-Alpha (TNF), 8-hydroxy-2'-deoxyguanosine (8‐OHdG), monocyte chemoattractant protein-1 (MCP-1), and Vascular Endothelial Growth Factor (VEGF) A were obtained at the pre and post time points and analyzed with Enzyme Linked Immuno-Assays (ELISA). Data were summarized with descriptive statistics.
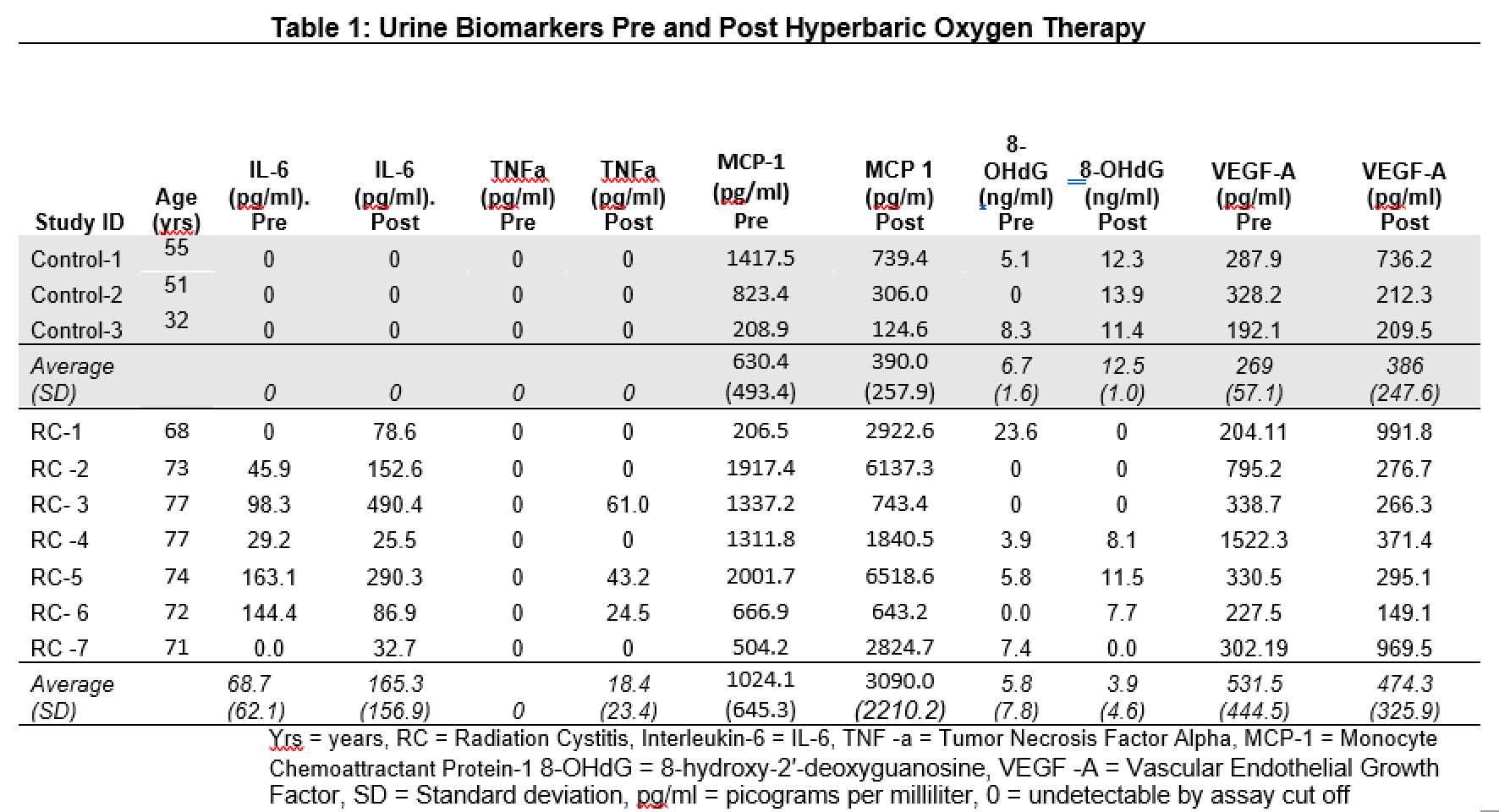
RESULTS: A total of 7 male patients, average age 73(SD±3), with severe radiation cystitis following radiation for prostate cancer and 3 controls met inclusion criteria. RC participants underwent an average of 49 HBO2 treatments. Urine biomarker results are detailed in Table 1. Urine IL-6 was uniquely elevated in RC patients pre-HBO2 and increased post-HBO2, however remained undetectable in controls. Urine MCP-1 was detected in control urine samples but found in higher concentration in the RC cohort and increased post-HBO2. TNF alpha was undetectable in both RC and controls prior to HBOT, however increased for some RC patients following treatment. Urine 8-OHdG and VEGF-A concentrations were variable in both RC patients and controls.
CONCLUSIONS: We determined urine collection and analysis is feasible pre and post-HBO2. Further, we found preliminary evidence that RC patients undergoing HBO2 have elevated baseline IL-6 compared to controls which increased in concentration following HBO2 course. MCP-1 was elevated in the cystitis cohort at baseline and increased following HBO2. In contrast, TNF-alpha, while undetectable in both RC participants’ baseline urine and controls per our assay parameters, increased in a proportion of RC patients post HBOT. IL-6, MCP-1, and TNF-alpha may be unique urine biomarkers to follow HBO2 outcomes. Further work is needed to elucidate these findings in larger cohorts.