BACKGROUND: Current evidence supports obtaining magnetic resonance imaging (MRI) prior to prostate biopsy (PMID 31642740). Potential deliverables of MRI include (1) improving detection of clinically significant prostate cancer (csPCa) through targeting of MRI lesions and (2) reducing the number of biopsies required by eliminating the need for systematic (i.e. non-targeted) biopsy. Prior research demonstrated the efficacy of the Actionable Intelligence Metric (AIM) and Reduction Metric (ReM) in quantifying these two deliverables; however, this work was done in the traditional transrectal biopsy setting. Recently, there has been renewed interest in transperineal prostate biopsy (TP-B). We assessed AIM and ReM in a large, multi-institutional cohort of men undergoing TP-B.
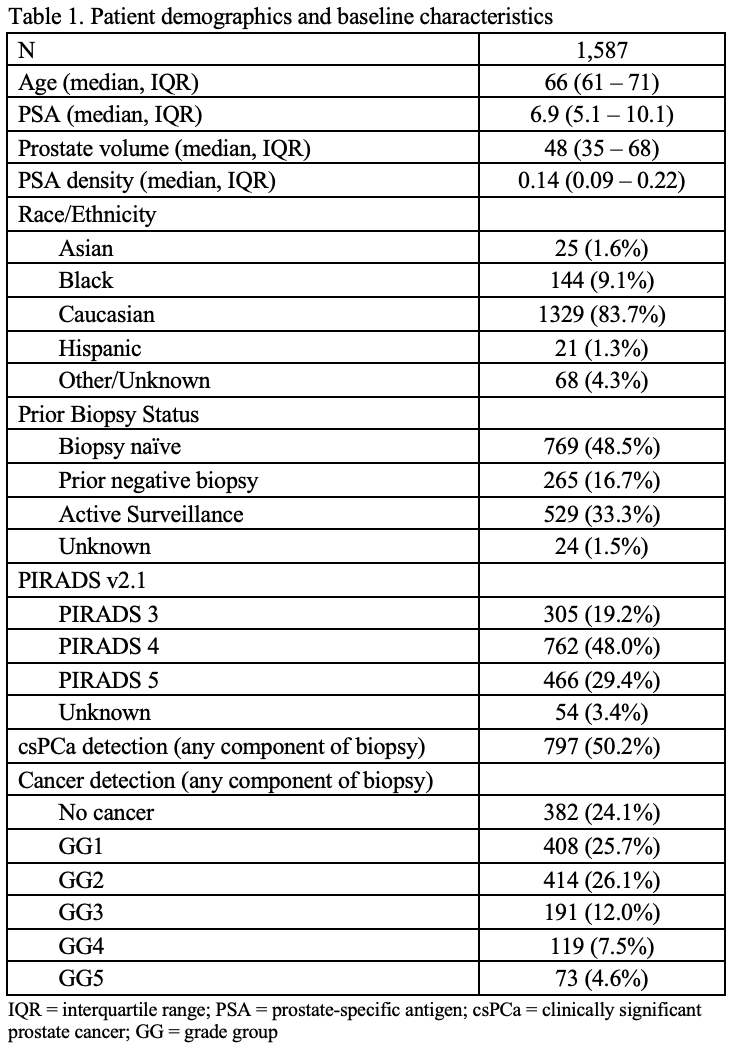
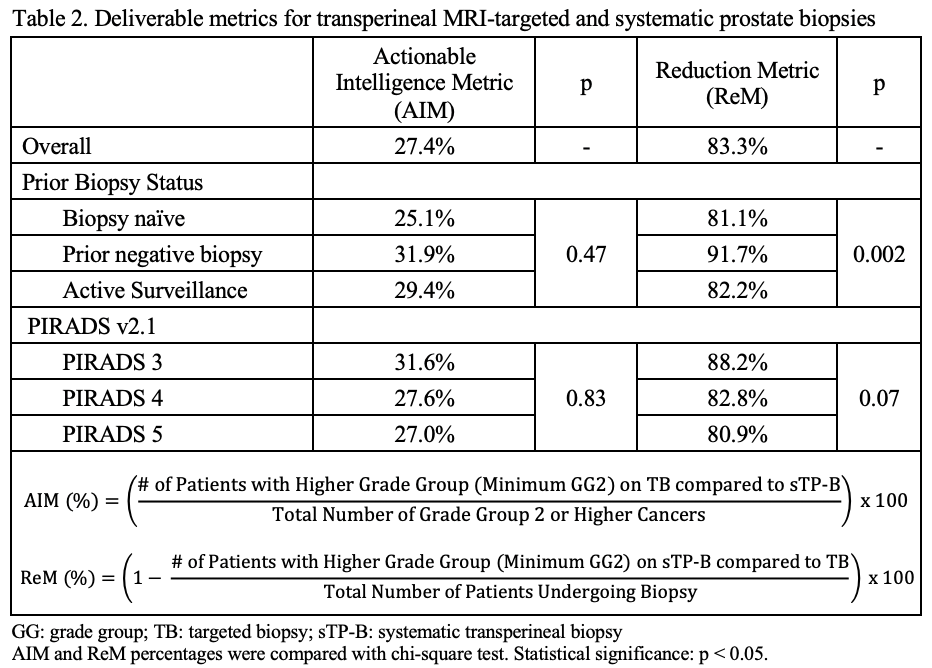
METHODS: All patients undergoing concurrent MRI/ultrasound (US) fusion targeted (TB) and systematic TP-B (sTP-B) and maintained in prospective prostate cancer databases across five institutions were included. csPCa was considered grade group (GG) ≥ 2. AIM is the percent of men in whom TB detected a higher GG compared to sTP-B alone (Table 2). ReM is the proportion of men in whom sTP-B may be omitted. Men were stratified by biopsy indication - biopsy na´ve, prior negative biopsy (PNB), or active surveillance (AS) and by PIRADS score (3-5).
RESULTS: 1,587 TP-B were analyzed; 797 (50.2%) had ≥GG2 PCa. Table 1 lists demographic and cancer detection data. AIM in the overall cohort was 27.4%, and ReM was 83.3%. When stratified by PIRADS score and AS/prior biopsy status, AIM and ReM were >25% and >80% respectively across all subgroups (Table 2). Values were highest for patients with a PNB and for those with a PIRADS 3 lesion.
CONCLUSIONS: AIM and ReM can be applied in the TP-B setting to assess deliverables of MRI/US fusion prostate biopsy. TB provides actionable information in 27% of men while ReM highlights that up to 17% of csPCa would be missed if sTP-B is omitted. Individualized assessment of patient risk tolerance is necessary if a TB alone approach is to be adopted.