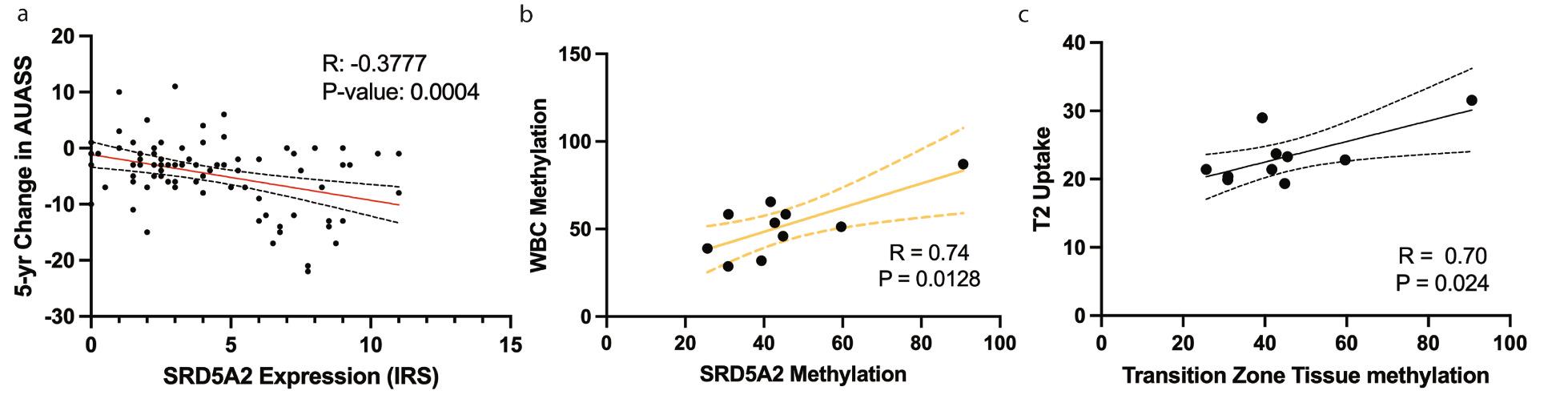
INTRODUCTION AND OBJECTIVE: Benign prostatic hyperplasia (BPH) is a common condition in men worldwide. Finasteride, which acts on the SRD5A2 receptor, is a mainstay for BPH treatment; however, not all men demonstrate a clinical response to finasteride and predictors of patient response are lacking. Inflammation has been linked to methylation of the SRD5A2 promotor and decreased expression. This study seeks to define non-invasive methods evaluating SRD5A2 methylation that can be utilized as biomarkers to predict therapeutic response to finasteride. METHODS: Prostate biopsy tissue and clinical data from the MTOPS trial patients were obtained (n=83), and SRD5A2 expression in prostate tissue was quantified by immunostaining. Patients from the MTOPS cohort were classified as good responders or poor responders based on a 3-point improvement on the American Urological Association Symptom Score (AUASS). Separately, blood, surgical prostate specimen, and MRIs were obtained from participants in a clinical trial at our institution (NCT04288427) (n=11). Prostate inflammation was quantified using ferumoxytol- enhanced MRI and prostate tissues were immunostained for SRD5A2. RESULTS: Using the MTOPS samples, we found that men who demonstrated good clinical response to finasteride had a higher SRD5A2 protein expression (p= 0.036), while poor clinical responders had lower SRD5A2 expression (Fig. 1a, R= -0.38, p= 0.0004). From our institutional cohort, SRD5A2 protein expression was negatively correlated with TZ prostate tissue methylation (R= -0.84, p= 0.0012). SRD5A2 methylation from transition zone (TZ) prostate tissue was directly correlated with a patientís peripheral WBC methylation (Fig. 1b, R= 0.74, p= 0.0128). In addition, TZ SRD5A2 methylation directly correlated with ferumoxytol uptake on patient MRI (Fig 1c, R=0.70, p=0.024). CONCLUSIONS: Our data suggest that SRD5A2 can be a useful marker to predict response to finasteride therapy. Prior to initiation of therapy, assessment of peripheral WBC methylation for SRD5A2 or ferumoxytol enhanced prostate MRI inflammation
evaluation can serve as non-invasive techniques to predict response to finasteride treatment.