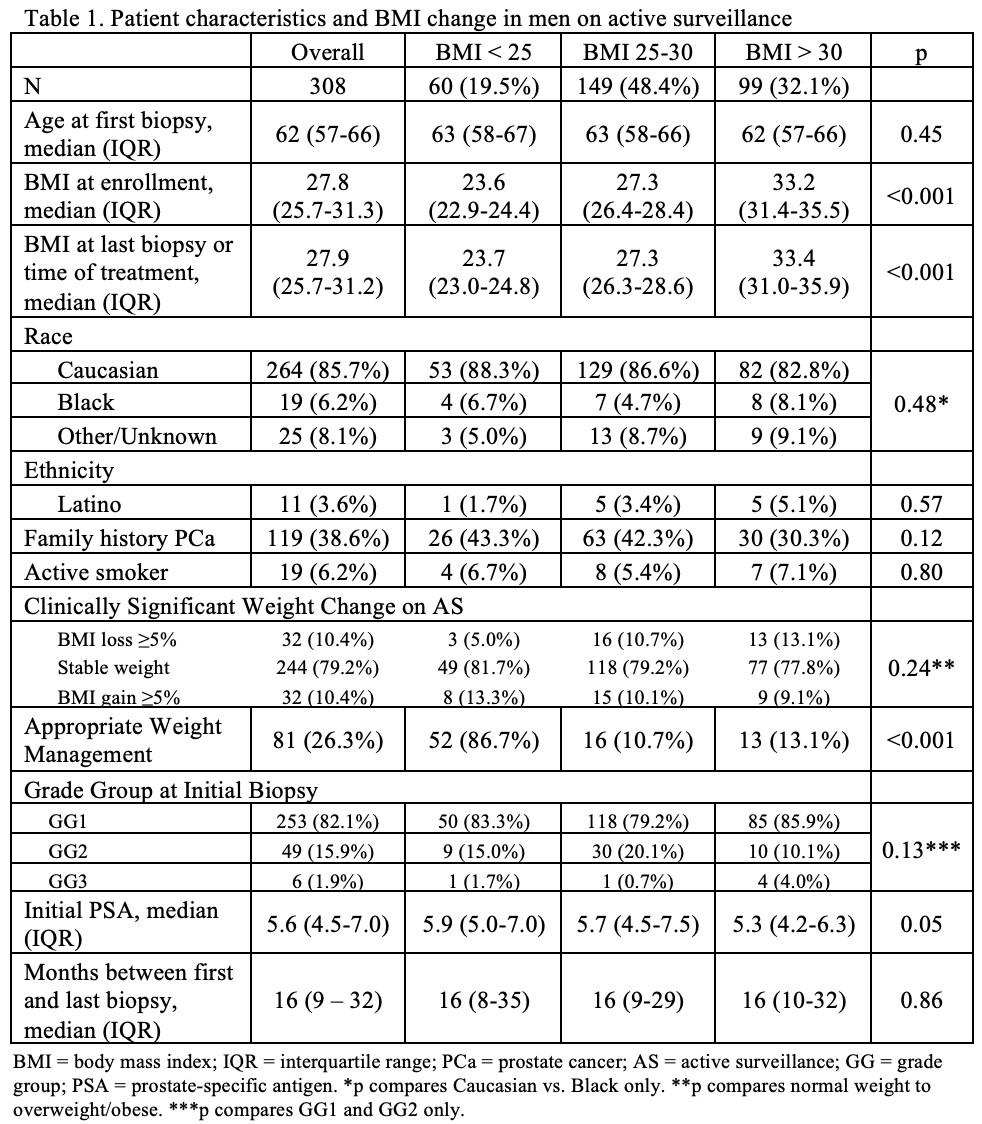
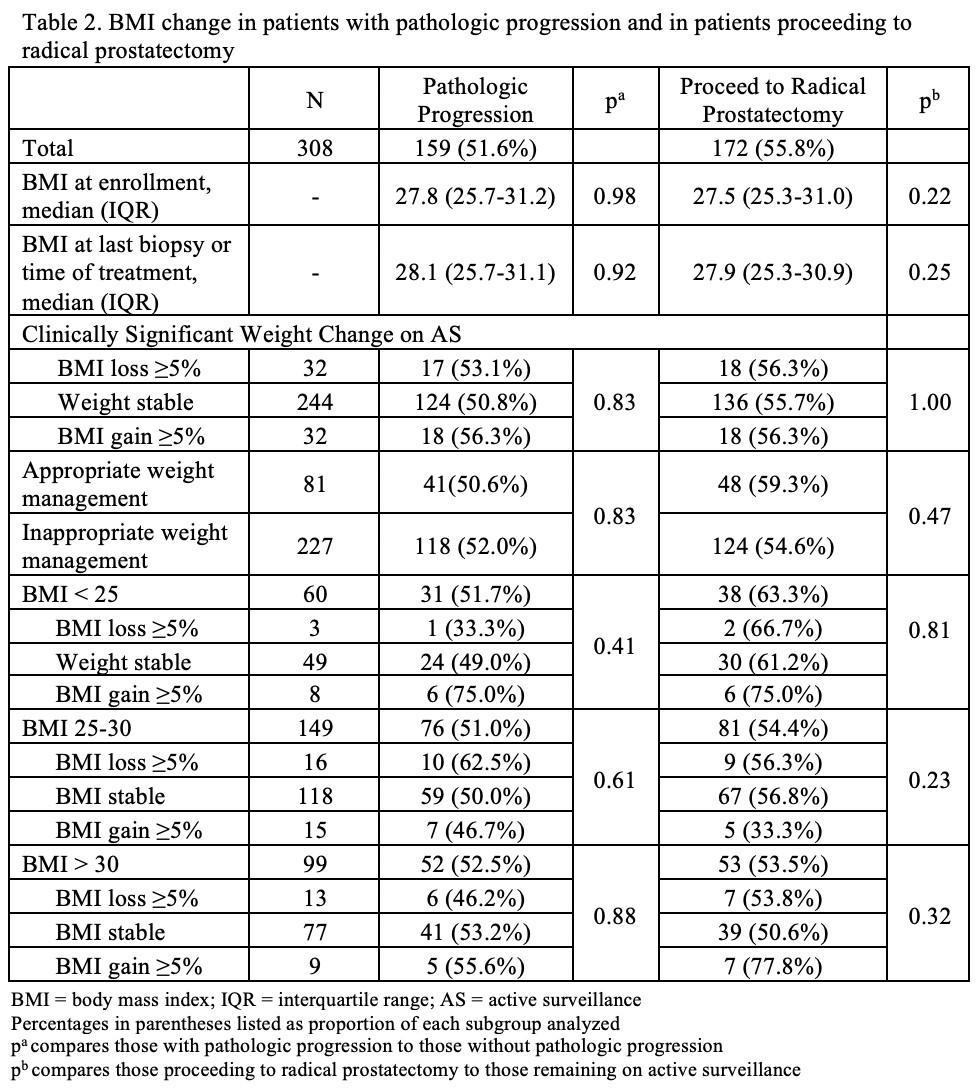
BACKGROUND: Patients classified as obese have worse oncologic outcomes on active surveillance (AS); randomized data suggest improved outcomes through intensive diet/lifestyle coaching. At our institution, AS patients are counseled on diet/lifestyle changes for general health and improved outcomes for potential future interventions. Our objective is to evaluate changes in body mass index (BMI) in men on AS and identify any association with oncologic outcomes. METHODS: A prospectively maintained AS database was queried for all men aged 18-89 initiating AS between 8/2016-3/2022 with at least 2 biopsies (PBx) at least 3 months apart. We evaluated differences in BMI change associated with Gleason grade group progression (GGP) and in men proceeding to radical prostatectomy (RP). Clinically significant (CS) weight change (WC) was defined as BMI change ≥5%. Appropriate weight management (AWM) was defined as CS weight loss in patients in overweight (BMI 25-30) or obese (BMI>30) categories and no weight gain in patients with BMI<25. GGP was defined as any Gleason grade group increase. RESULTS: 308 patients were evaluated (Table 1), of whom 159 (52%) had pathologic progression and 172 (56%) underwent RP (Table 2). 21% had CS WC, with equal proportions losing and gaining CS weight. Patients had similar rates of weight loss, gain, and maintenance regardless of initial BMI status. Neither WC nor AWM had a significant association with GGP or progression to RP (Table 2). Of men undergoing RP, 15/135 (11%) with BMI >25 had CS weight loss between final PBx and RP over a median time of 3 months. CONCLUSIONS: Despite counseling, CS weight loss is uncommon in patients on AS. CS WC was not associated with GGP in our cohort. Compared to men remaining on AS, patients in overweight/obese categories who proceeded to RP did not demonstrate greater CS weight loss even after their final biopsy despite having the most incentive to lose weight. The high proportion of patients classified as overweight/obese (81%) and patients proceeding to RP (56%) highlights the need for more intensive weight management strategies for those on AS.