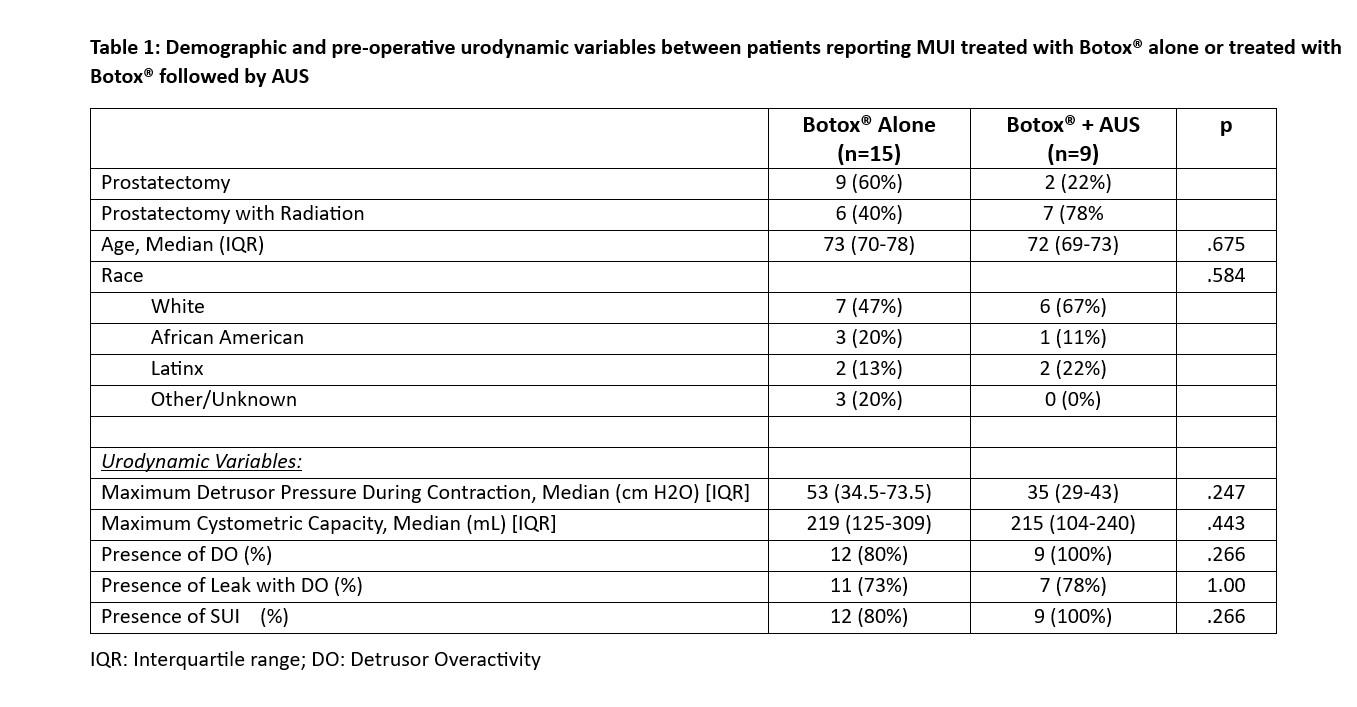
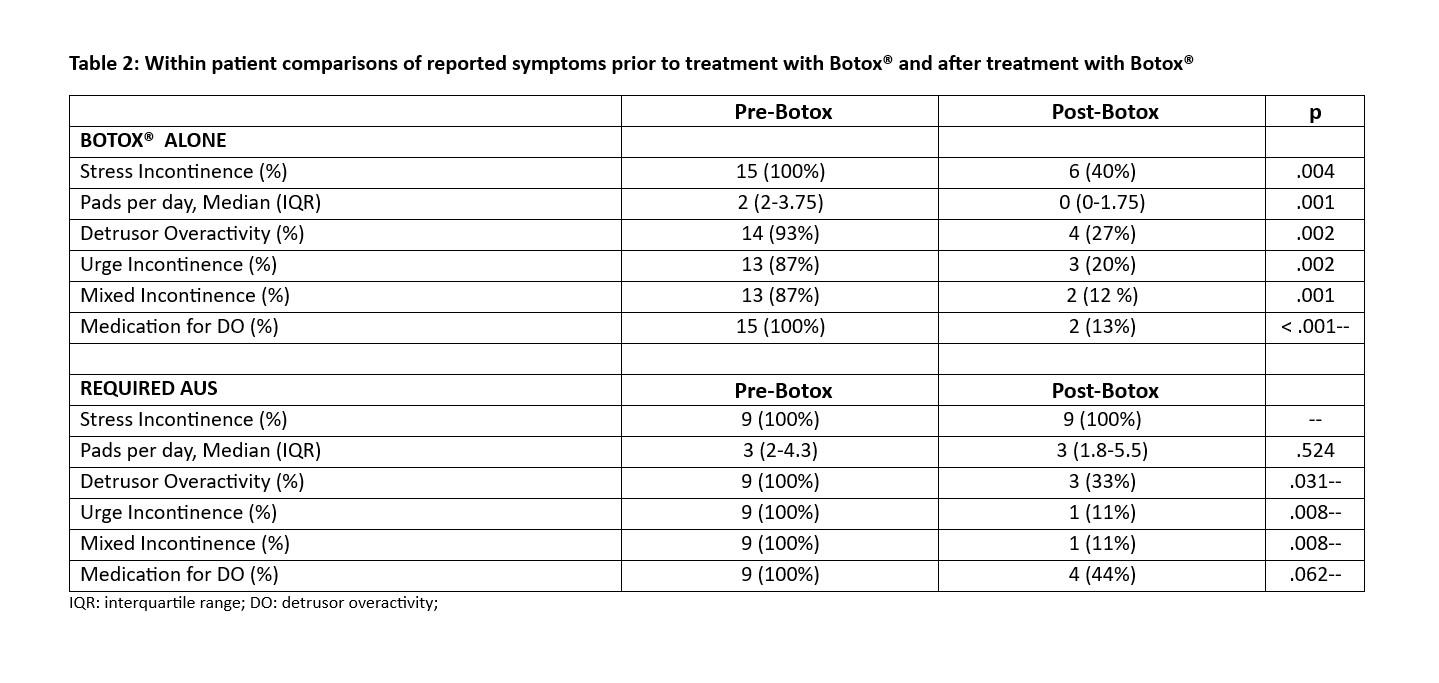
BACKGROUND: Deciding whether to initially target stress (SUI) or urge incontinence (UUI) for patients with mixed urinary incontinence (MUI) after radical prostatectomy (RP) is a challenging task. Studies have suggested artificial urinary sphincter (AUS) produces the best functional outcomes even when urodynamics (UDS) reveals MUI. We hypothesized that a subset of men with MUI after RP may be successfully treated with Botox® alone, avoiding the need for an anti-SUI procedure. METHODS: We retrospectively identified men (ages 18-89) who received Botox® after RP between 2016-2023. All patients underwent a prostatectomy with or without salvage/adjuvant radiation. Two groups were identified: men treated with Botox® alone and men requiring AUS placement after Botox®. The primary outcome was symptomatic improvement of incontinence after Botox®. Urodynamics and pre/post-Botox® symptoms were compared between and within groups, respectively, using Chi-squared, Fisher’s exact test, Wilcoxon rank sum tests, Wilcoxon signed rank and McNemar tests. RESULTS: Twenty-four men met inclusion criteria (Table 1). All but two (92%) reported MUI on symptom assessment in the office. The two patients without MUI complained of SUI on symptom assessment but were also found to have UUI on UDS. 15 patients (63%) were successfully treated with Botox® alone. 9 patients (38%) underwent AUS placement after Botox® for persistent SUI. 100% of patients who required an AUS had persistent SUI after Botox®. Interestingly, 9 men (60%) treated with Botox® alone no longer reported SUI after treatment. Patients treated with Botox® had significant improvement in most reported symptoms on follow up (Table 2), including 8 who were deemed pad free. None required clean intermittent catheterization after treatment. CONCLUSIONS: A subset of men with MUI after RP may be managed with Botox® alone. Identification of UUI-predominant MUI and/or the presence of DO on UDS aided in the decision to pursue Botox® as initial therapy. The potential to avoid AUS placement substantially improves quality of life for this subset of patients.