BACKGROUND: The role of serial tissue-based gene expression (genomic) testing among patients managed with active surveillance (AS) for localized prostate cancer is unclear. We aimed to examine patterns of serial genomic testing with the Decipher genomic classifier (GC) and assess the relationships between changes in GC and short term clinical outcomes.
METHODS: We performed a retrospective analysis of patients on AS for prostate cancer who underwent GC testing on at least two distinct prostate biopsies occurring between January 2017 and May 2023. The primary study objective was to assess the association between changes in GC and Gleason grade group (GG) upgrade during surveillance. Among the subset of patients who were treated with radical prostatectomy (RP), we evaluated the relationship between GC changes and the detection of adverse pathology (GG ≥3 and or pT3a or N1).
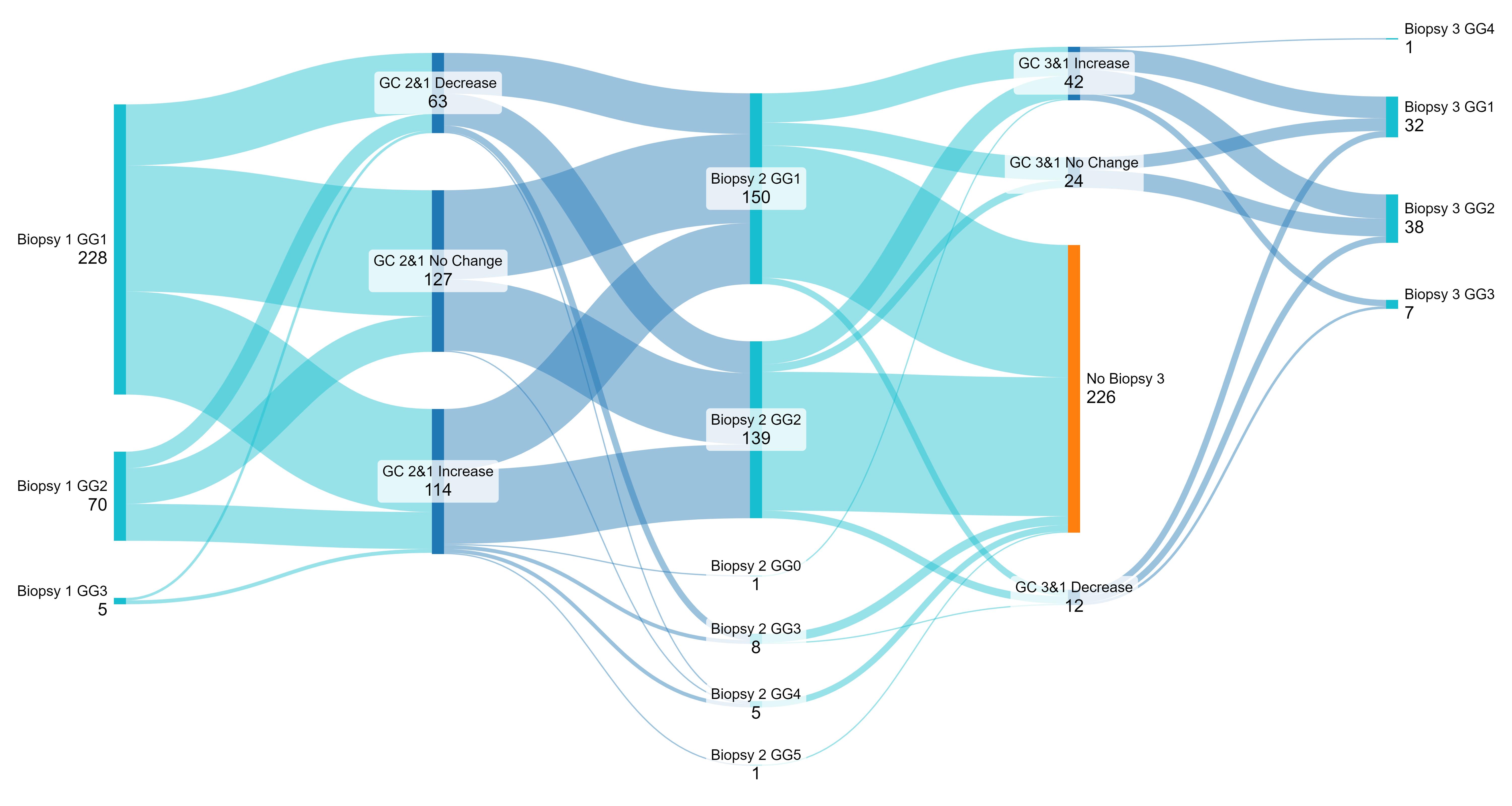
RESULTS: We identified 303 patients enrolled in AS for GG1 (n=228, 75.2%), GG2 (n=70, 23.1%), or GG3 (n=5, 1.7%) prostate cancer who received serial GC testing. GC scores decreased by at least 0.1 from the first to the second biopsy in 63 (20.7%) patients on AS, increased by at least 0.1 in 114 (37.5%), and did not change in 127 (41.8%) (Figure 1). The median change in GC scores was 0.04, (interquartile range, IQR -0.06 to +0.17). Increases in GC of at least 0.1 were observed in 80 (35.2%) patients with biopsy GG1 on initial biopsy, 29 (41.4%) with GG2, and 0 patients with initial GG3 disease (p=0.03). Among 78 patients who underwent a third prostate biopsy, Gleason upgrade occurred in 42 (53.8%), no change greater than 0.1 in 24 (30.8%), and downgrade occurred in 12 (15.3%). In univariable logistic regression, GC increase (OR 3.067, 95% CI 0.97-9.737, p=0.057) was not significantly associated with Gleason upgrade. Additionally, patients were separated into different risk groups: GG1 and very low risk decipher <0.2; GG1 and decipher 0.21-0.44; GG1 and decipher >0.45 or GG2 and decipher <0.45; GG2 and decipher >0.45 or higher or GG3 with any decipher. These risk groups did not have significant odds of GC increase or Gleason upgrade. The only significant association with the initial GC category (low, intermediate, and high risk) was lower odds of GC increase when the initial GC category was high (OR .179, p=0.24). Initial GC category was not associated with Gleason upgrade. Adverse pathology was identified in 14 of 51 (28%) patients treated with RP of whom the median change in Decipher score was +0.03, compared with +0.04 of those with favorable pathology (p=0.73).
CONCLUSIONS: Among patients undergoing Decipher GC testing during AS for prostate cancer, there was substantial variation in serial test results; however, increases in GC were not associated with short-term biopsy upgrade.