Background: Prompt timing of radical cystectomy (RC) following diagnosis of muscle invasive bladder cancer (MIBC) is important, with a delay beyond 12-weeks traditionally considered to impart worse oncologic outcomes. However, no randomized clinical trials have examined this question, and these recommendations are based on historical data. We therefore emulated a hypothetical target clinical trial using a contemporary, nationwide oncology dataset to evaluate the association of time from diagnosis to RC with oncologic outcomes.
Methods: We conducted observational analyses designed to emulate a hypothetical target trial of early versus late RC using the National Cancer Database from 2006-2015. Specifically, we identified adults age 40-79 years with incident cT2-4 N0 M0 urothelial carcinoma of the bladder, who did not receive neoadjuvant chemotherapy, treated with RC from 4-18 weeks following diagnosis. We defined “early RC’ and “late RC” as occurring before or on/after 12 weeks, respectively. After estimating a propensity score for treatment using logistic regression, we evaluated the association of late RC with pathologic upstaging at RC and overall survival (OS) with adjustment by stabilized inverse probability weights (sIPW). We also conducted exploratory analyses evaluating the association of time to RC with each outcome modeled flexibly, both as a linear continuous variable and using restricted cubic splines with 3 knots.
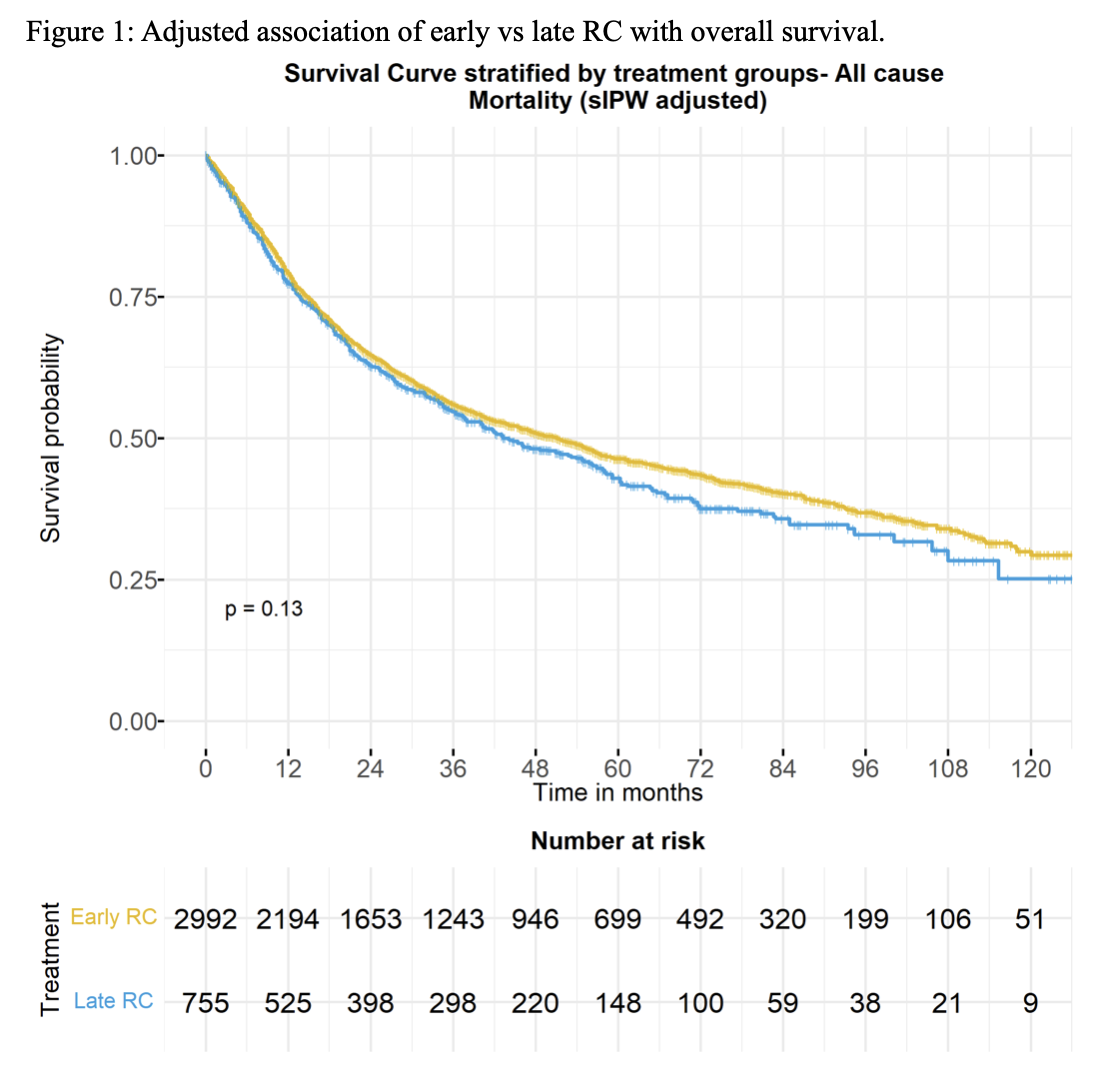
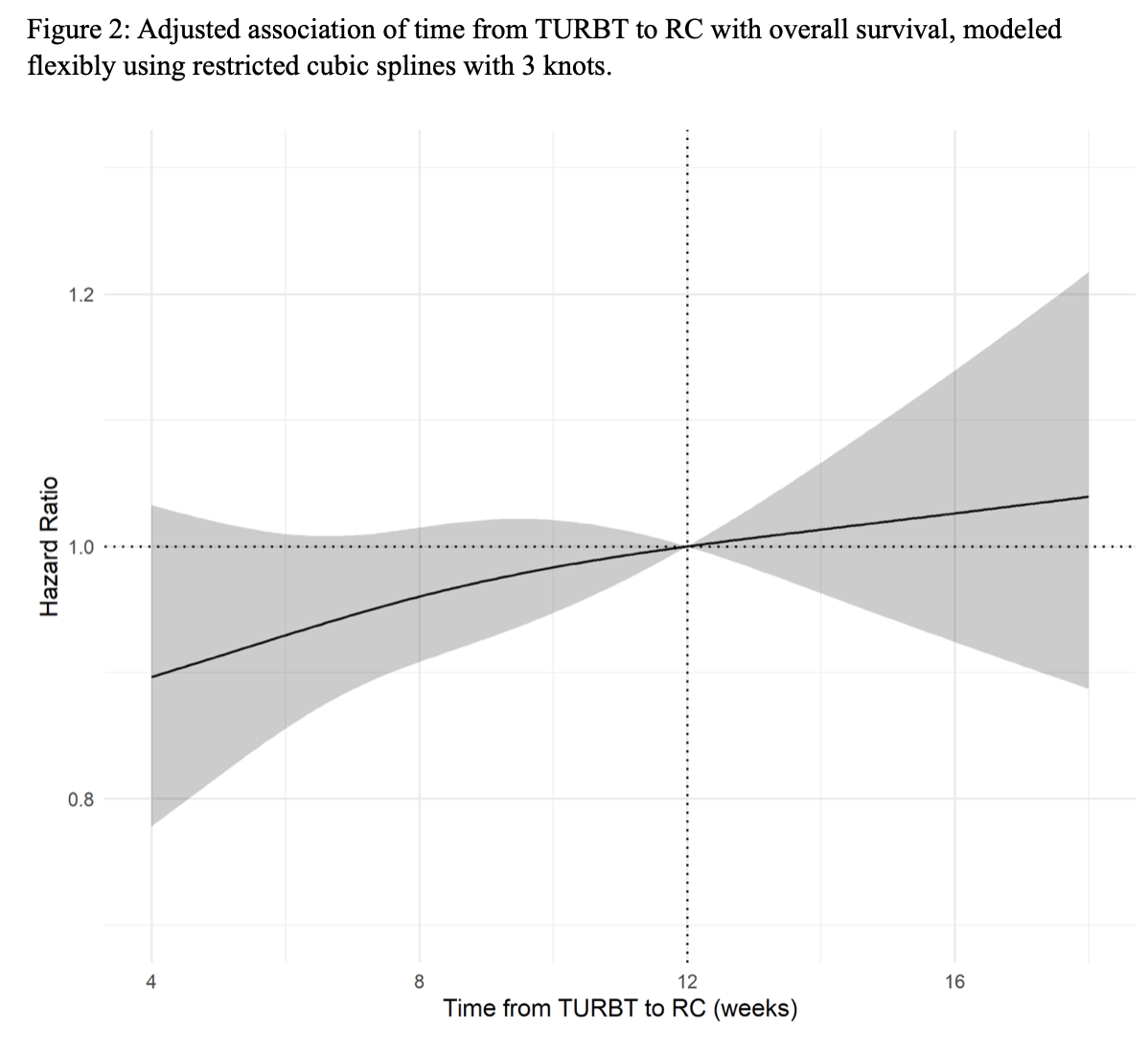
Results: A total of 3,747 patients were included for this study, including 2,992 who underwent early RC and 755 who underwent late RC. Baseline characteristics were well balanced after sIPW reweighting. Median follow-up was 28.1 months, and during follow-up 1,884 all-cause deaths occurred. In adjusted analyses, late RC was not associated with an increased risk of pathologic upstaging compared to early RC (48% vs 52%, p=0.07). Similarly, there was no statistically significant difference in adjusted OS, with 5-year OS of 43% vs 46% p=0.13 for late and early RC, respectively (Figure 1). Similar findings were observed across categories of cT stage, age, Charlson index, and gender. In exploratory analyses modeling time to RC flexibly, a longer time to RC was associated with a modest, approximately linear decrease in the adjusted risk of pathologic upstaging, and no statistically significant difference in OS (Figure 2).
Conclusion: In observational analyses designed to emulate a hypothetical target trial of early versus late RC, timing of RC was not associated with a statistically significant increase in pathologic upstaging or a difference in OS when performed from 4 to 18 weeks after diagnosis. These results suggest the need to examine the traditional recommendations for timing of RC following diagnosis.
Figure 1: Adjusted association of early vs late RC with overall survival.
Figure 2: Adjusted association of time from TURBT to RC with overall survival, modeled flexibly using restricted cubic splines with 3 knots.