Background Radical cystectomy (RC) with urinary diversion remains the gold-standard treatment for non-metastatic muscle-invasive bladder cancer (MIBC), yet it carries significant morbidity and mortality. RC has the highest rate of 90-day readmissions (40%) among all surgical oncologic procedures, and an estimated perioperative complication rate of 60%. Therefore, patients require data-driven perioperative risk assessment to frame expectations and guide postoperative management. The American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) Surgical Risk Calculator (SRC) is a commonly used tool to help determine which specific patient factors are likely to contribute to their personal risk framework. However, the value of the NSQIP-SRC in prognosticating complications following RC for MIBC remains uncertain. This study aims to evaluate the accuracy of the tool in predicting RC postoperative complications.
Methods A prospective cohort of patients undergoing RC from 2020-2023 at a single-institution, tertiary medical center was retrospectively reviewed. The NSQIP-SRC-predicted 30-day probabilities of postoperative complication (any complication, serious complication, readmission, mortality) were compared with actual rates. The NSQIP-SRC’s predictive value was examined with Receiver Operator Characteristic (ROC), Area Under the Curve (AUC) C-statistic, and Brier scores.
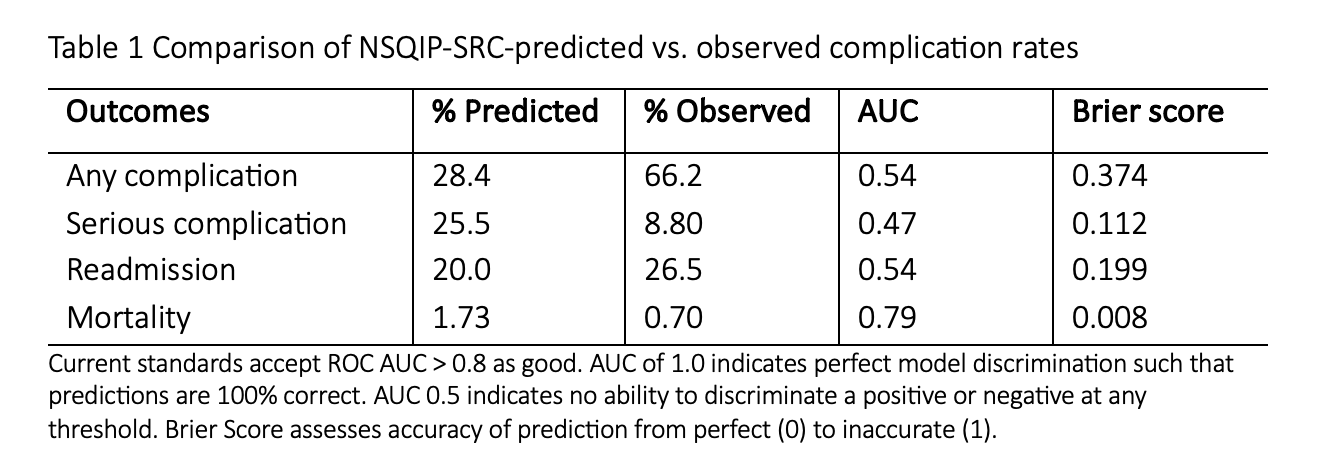
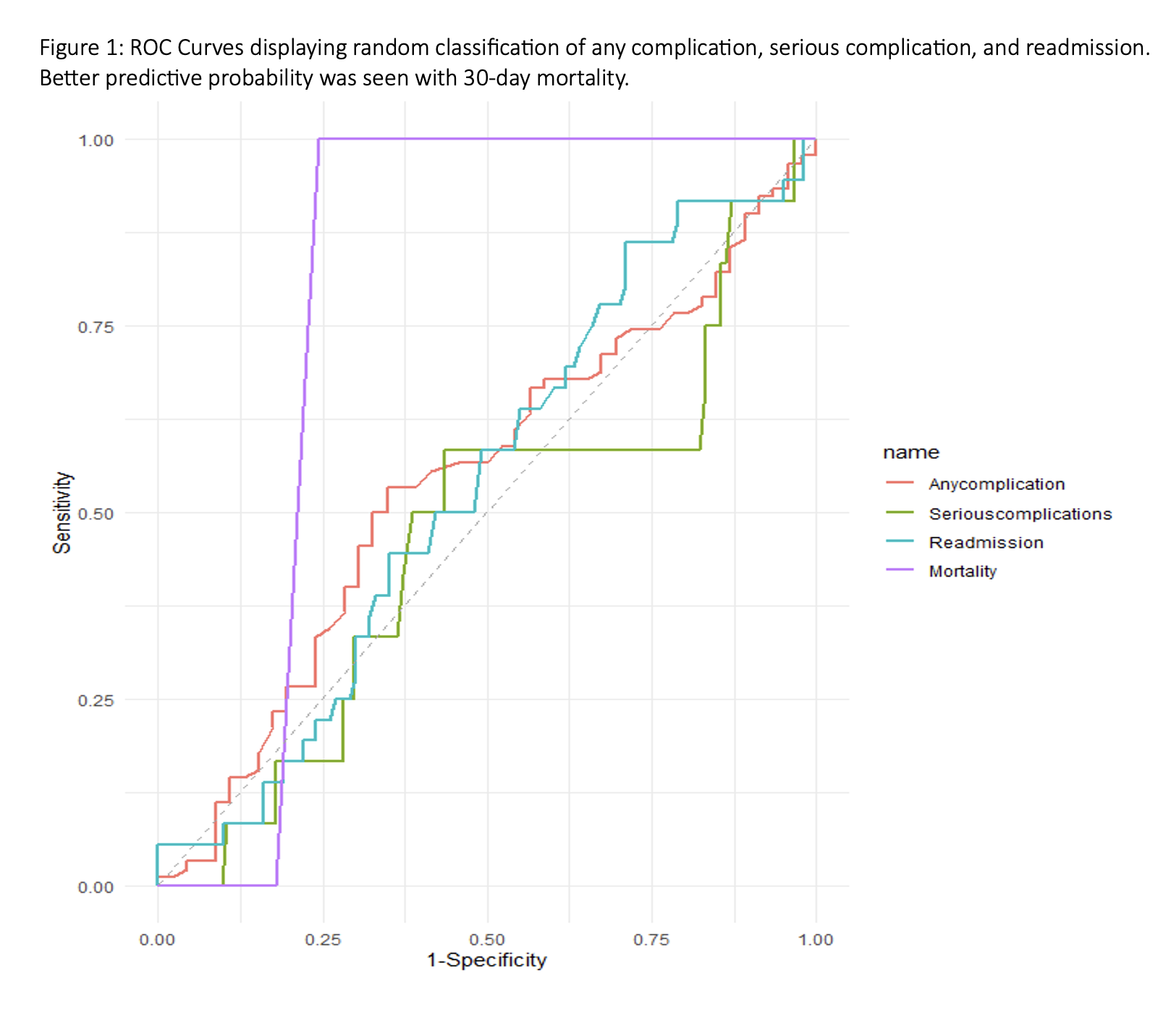
Results A total of 136 patients were included in analysis. There was significant discordance between the rate of NSQIP-SRC predicted vs. observed complications with NSQIP-SRC overestimating serious complication while underestimating any complication probability (Table 1). ROC shows prediction to be no better than random chance for any complication, serious complication, and readmission with AUC < 0.54 for all three risk categories (Figure 1). AUC and Brier scores confirm a near perfect prediction of random chance for NSQIP-SRC prediction of serious complication, any complication, and readmission. 30-day mortality approaches acceptable threshold for predictive probability, AUC 0.79. NSQIP-SRC self-reported AUC is 0.82, which was not demonstrated in our patient population.
Conclusions The NSQIP-SRC is a poor predictor for surgical outcome among patients undergoing RC. Counseling based on the NSQIP-SRC is no better than a coin toss and may serve to mislead patient understanding about their own personal risk regarding this morbid surgical procedure. Limitations in NSQIP methodology specific to RC may underlie this lack of utility and there remains an opportunity and need to develop institution-specific risk calculators.