BACKGROUND: Radical Cystectomy (RC) remains the gold standard treatment for invasive bladder cancer. Although approximately 20% of patients treated with RC are female, their health-related quality of life (HRQOL) outcomes have not been well characterized. Our objective was to describe HRQOL at baseline in the female cystectomy population and then in the 24 months following surgery. Next, we compared both their baseline and postoperative HRQOL to the male cohort.
METHODS: Subjects enrolled in a prospective study of RC HRQOL at Memorial Sloan Kettering from 2008-2014 were analyzed. This included the entire 411-subject cohort (80% male, 20% female) who completed 14 validated HRQOL measures preoperatively and at 3, 6, 12, 18, and 24-months post-RC. We analyzed measures of general cancer-related (EORTC QLQ-C30) and bladder cancer-specific QOL (EORTC QLQ-BLM30), Bowel function (MSKCC BFI), urinary (AUA Symptom Score, IIQ, UDI), and several measures of psychosocial QOL. First, we compared baseline pre-surgical differences in HRQOL between female patients that later underwent continent (orthotopic neobladder or continent cutaneous diversion) versus ileal conduit urinary diversion using a two-sample t-test. Generalized estimating equation (GEE) models were then used to illustrate scores over time separately in female ileal conduit and continent diversion cohorts. Next, we used GEE models to compare baseline HRQOL between female and male patients, and a second model compared mean post-RC scores.
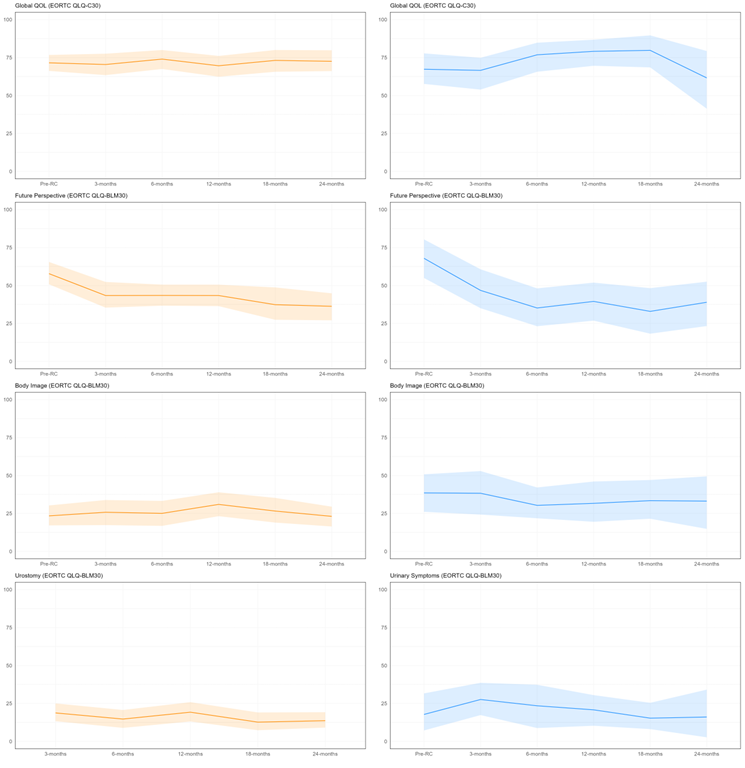
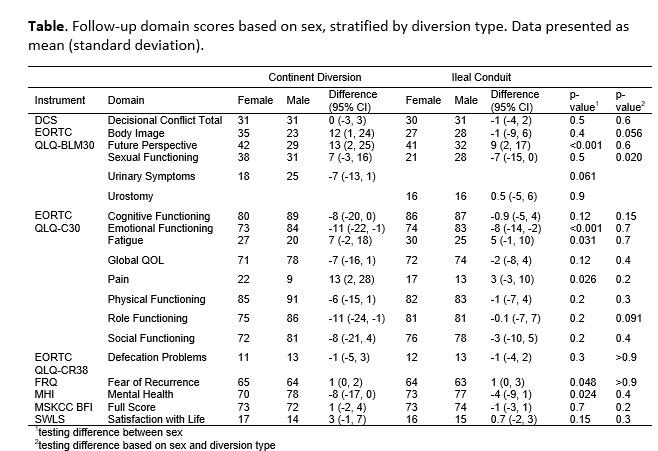
RESULTS: In this sample, 88 (21%) were female, of which 73% underwent ileal conduit urinary diversion. Preoperatively, women undergoing continent diversion had lower Social Functioning scores (mean difference 18; 95% CI 0.30,35, p=0.046), but did not differ in Global QOL or Physical Functioning. Baseline Body Image scores were higher (worse) among continent diversion patients (mean difference -15; 95% CI -29,-1.0, p=0.037). The Figure shows selected HRQOL domains separately in female ileal conduit (orange) and continent diversion (blue) cohorts. In both, Global QOL remained stable from preoperatively to 24-months. Future Perspective, with higher scores equaling worse fears about the future, improved meaningfully (>20 points) in both groups by 6 months. Body Image scores did not worsen in either cohort postoperatively. Urostomy and Urinary Symptom scores (in ileal conduit and neobladder patients, respectively) were slightly worse at 3 months, then gradually improved. In comparison to male patients, female patients had worse baseline Emotional Functioning (p<0.001), Social Functioning (p=0.033), Mental Health Inventory (p<0.001), Future Perspective (p=0.001), Body Image (p=0.011), and Sexual Functioning (p<0.001) scores. Postoperatively, these trends generally continued with worse Emotional Functioning (p<0.001), Future Perspective (p<0.001), and Mental Health Inventory (p=0.024) scores (Table). Notably, Pain (p=0.026) and Fatigue (p=0.031) were also worse in women.
CONCLUSIONS: Female HRQOL after radical cystectomy was generally favorable, however, there was evidence that emotional/psychosocial domains were worse at baseline in the female RC population and this effect continued postoperatively.