BACKGROUND: The use of single-port (SP) robotic surgery within the urology community has been rising despite a lack of comparative effectiveness with the standard approach using the multi-port robotic system. We compared perioperative outcomes between SP and multi-port (MP) robot-assisted partial nephrectomy (RAPN).METHODS: Data from all SP and MP retroperitoneal and transperitoneal RAPN from August 2009 to February 2024 were obtained from our prospectively mantained institutional database. Propensity-score matching (PSM) was performed using '1:2 nearest neighbor' matching method (discard = control group, caliper = 0.2). Patients were matched for age, gender, race, BMI, Charlson score and tumor size. Our primary outcome was to compared perioperative outcomes between the SP and MP group.
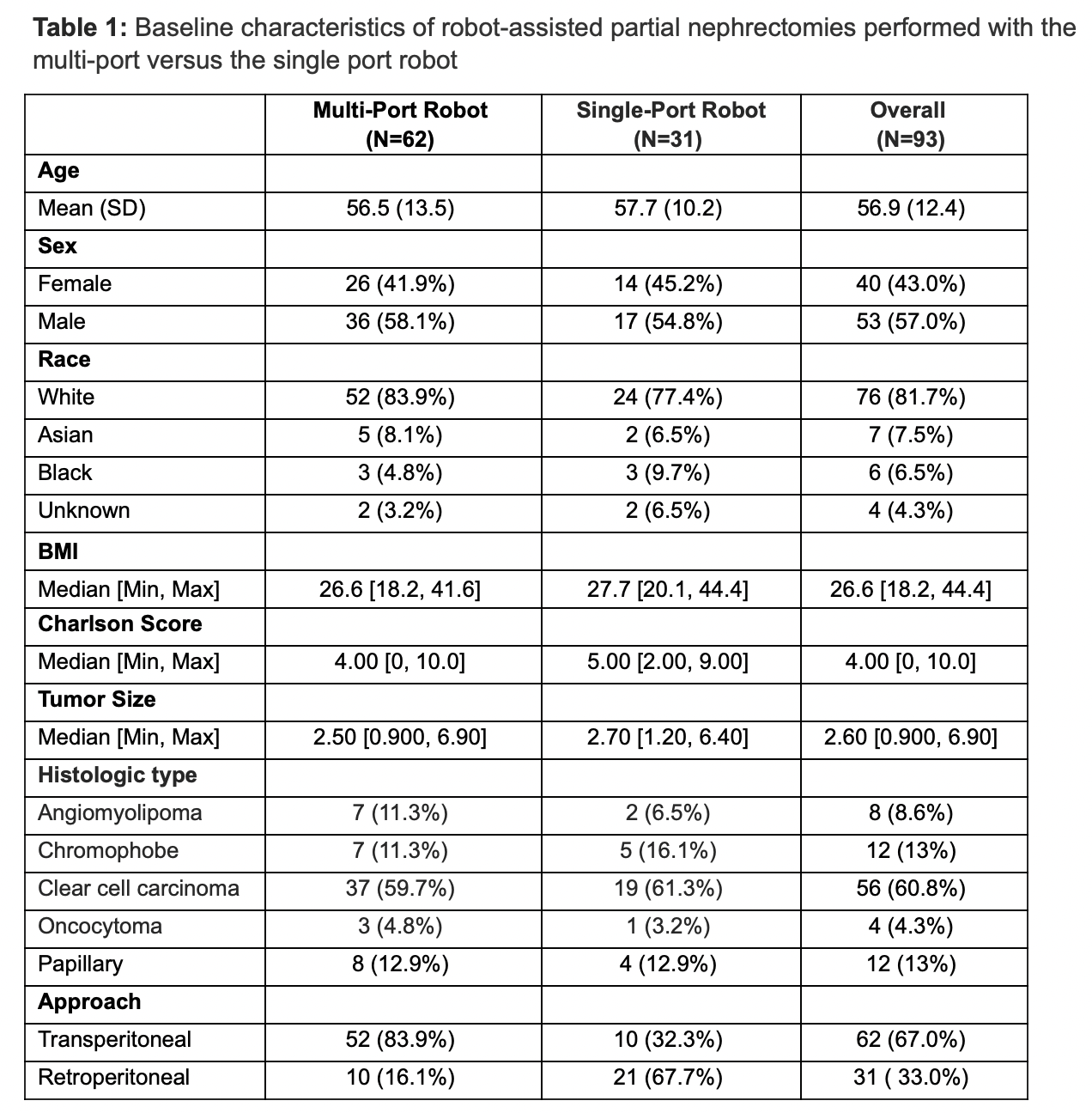
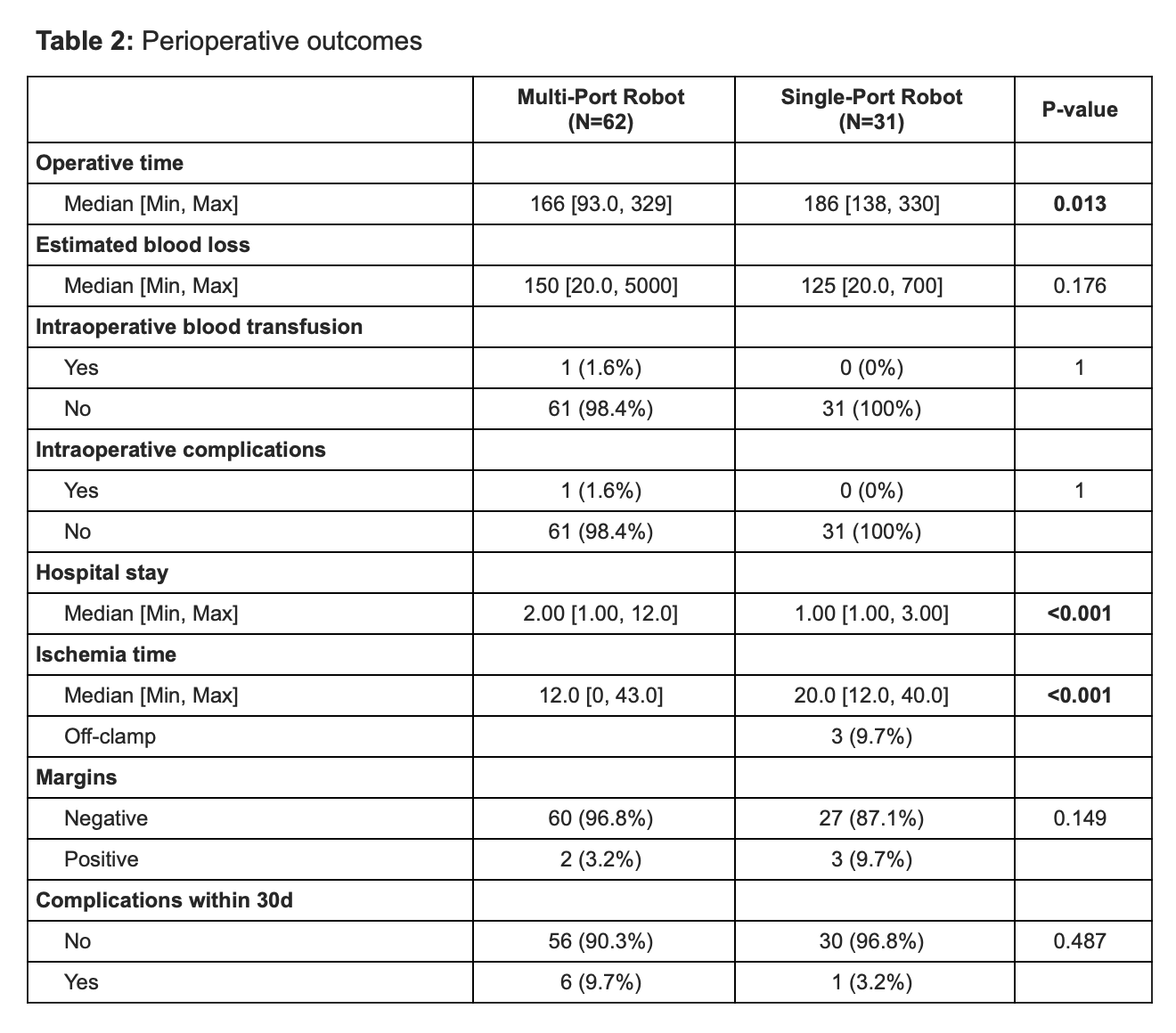
RESULTS: A total of 839 RAPNs were performed by 2 surgeons during our study period. After PSM, 31 SP cases were matched to 62 MP cases (tables 1-2). In the SP group, 68% of the cases were done via a retroperitoneal approach, in contrast to the MP group where 16% were retroperitoneal. One case was converted to open surgery in the MP group. The operative time was longer in the SP group compared to the MP group (186 min vs 163 min, p-value: 0.01). Patients who underwent SP-RAPN had a shorter median length of hospital stay (1 day vs 2 days, p-value: < 0.001). Three SP cases were performed off-clamp however overall, the MP group had a shorter warm ischemia time (12 min vs 20 min, p-value: < 0.001). In the SP group, there were 3 cases with positive margins, all of which were anterior or upper pole tumors performed retroperitoneally.
CONCLUSIONS: Based on our initial experience, SP RAPN appears to be a safe and feasible approach for cT1 tumors with perioperative outcomes comparable to those of MP RAPN. However, SP RAPN performed early in the learning curve has a longer operative and warm ischemia time than MP RAPN performed by an experienced team.