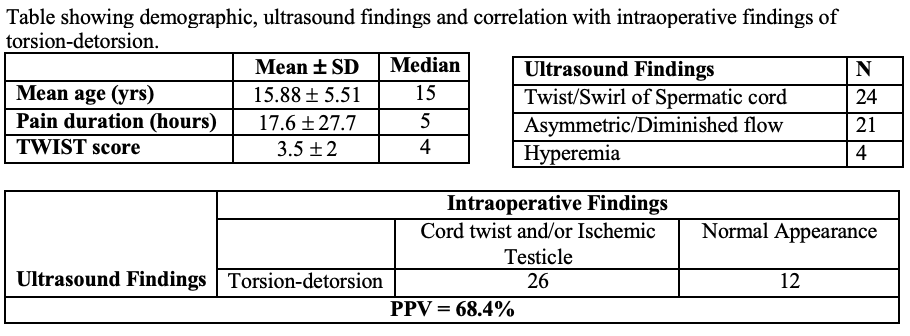
Background: Testicular torsion is a urological emergency, however there is clinical ambiguity associated with torsion-detorsion or intermittent torsion. In this study, we retrospectively analyzed patients who underwent immediate scrotal exploration in the setting of a diagnosis of torsion-detorsion to identify ultrasound predictors of those at greatest risk of testicular loss. Methods: We retrospectively reviewed all patients who presented to the emergency department of our tertiary hospital with concerns for testicular torsion between 2015 and 2023. Patients with history, physical exam or ultrasound findings described by radiologists suggestive of torsion-detorsion were further analyzed. Patient demographics, duration of pain, ultrasound and intra-operative findings and peri-operative outcomes were assessed. Results: A total of 169 patients were identified of which, 50 met inclusion criteria for torsion-detorsion and immediate exploration. The median age at the time of presentation was 15 years old. 2 patients had a known history of ipsilateral undescended testicle. Average hours of testicular pain prior to presentation were 17.6 hours (range 0 - 144 hours). Most common presentation, 49/50 patients, was testicular pain. One patient presented solely with a high riding testicle. Median TWIST score was 4. Most common ultrasound finding was twisting or swirl in the spermatic cord which was described in 24/50 patients, followed by asymmetric or reduced blood flow but not absent flow in comparison to contralateral testicle in 21/50 patients. Hyperemia was described in only 4/50 patients. All patients underwent scrotal exploration and bilateral orchidopexy on the day of presentation. 12/50 patients were manually detorsed prior to surgical fixation. Excluding manual detorsion in 12 patients, 26 ultrasound findings correlated with operative findings of at least 180 degrees twisting or congestion of the spermatic cord and/or discoloration of the ipsilateral testicle. The remaining patients had pink, healthy, and untwisted testicle. None of patients underwent orchiectomy. Only two patients had abnormal findings of asymmetric size of testicles on follow up after 2 weeks. Conclusions: Torsion-detorsion is a common radiographic diagnosis of acute testicular pain. Twisting or swirl in the spermatic cord was the most common ultrasound description. Ultrasound findings correlated with intra-operative findings with a positive predictive value of 68.4%. There was no testicular loss. Findings of twisting of the spermatic cord or asymmetric blood flow even in the presence of bilateral blood flow is a reasonable indication for scrotal exploration and bilateral orchidopexy to prevent testicular loss.