BACKGROUND: Endoscopic prostate surgery increases septic morbidity and mortality. While Urology guidelines discuss preoperative urine culture (UCX), it is ultimately left to the surgeonís discretion to obtain, generally influenced by factors such as experience, risk aversion, patient comorbidities, and patient presentation. We assessed the impact of preoperative UCX on postoperative urinary tract infection (UTI) risk among men who underwent endoscopic prostate surgery; and identified the patient-level factors associated with preoperative UCX testing.
METHODS: We queried the Veterans Affairs Surgical Quality Improvement Program between 2015-2022 for men who underwent benign prostate endoscopic procedures (transurethral resection of the prostate (TURP), laser enucleation, laser vaporization, or Re-TURP). Preoperative UCX was defined as within 30 days pre-surgery. The primary endpoint was postoperative UTI within 30 days. We fitted a multivariable logistic regression to examine the effect of preoperative UCX on postoperative UTI risk adjusting for veteran-level covariates and type of surgery. Second, we fitted a multivariable logistic regression to identify patient-level and surgery-specific factors associated with of preoperative UCX testing. Third, experimental event rate (UTI among those without preoperative UCX), control event rate (UTI among those with preoperative UCX), absolute risk reduction, and number needed to harm were calculated.
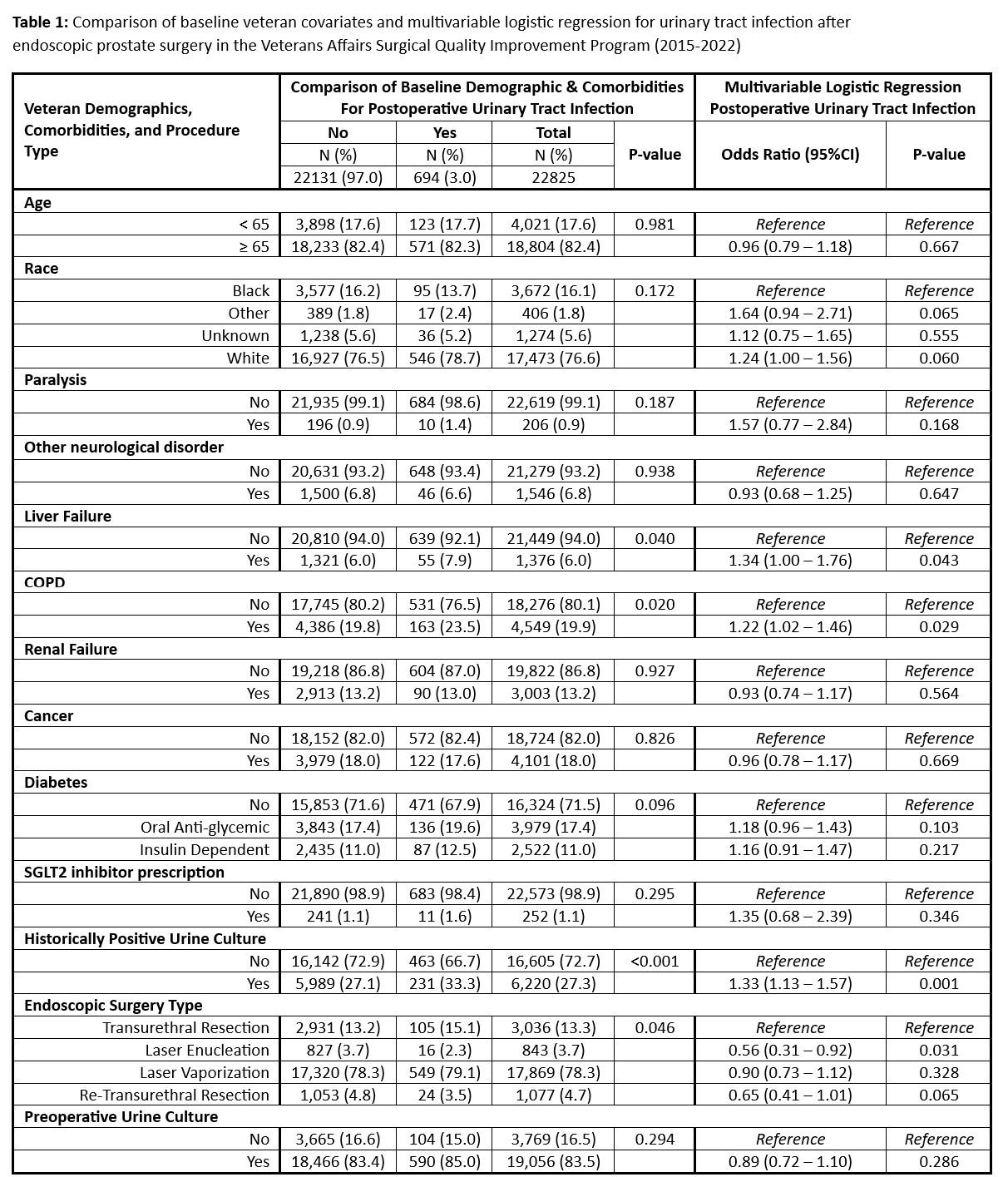
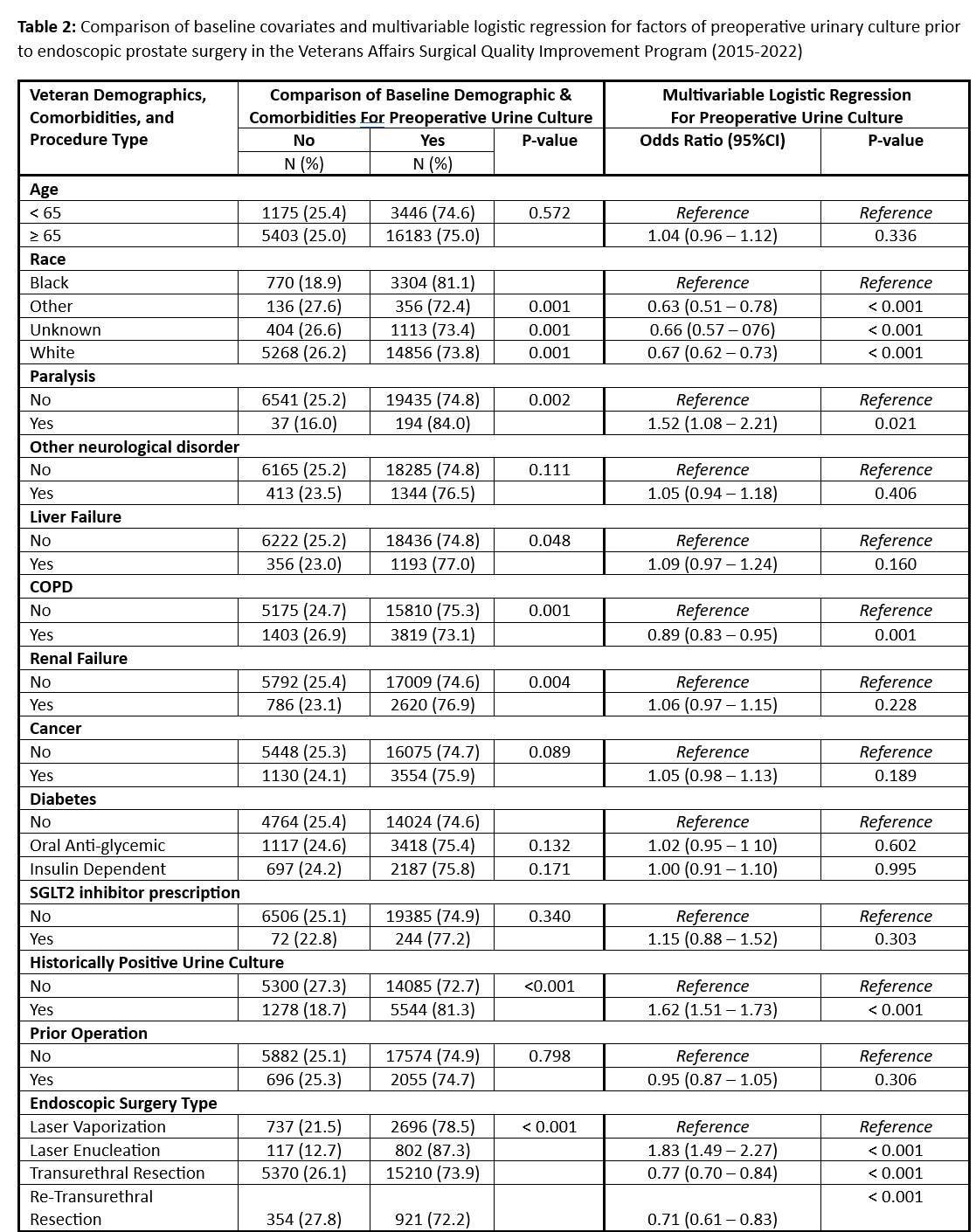
RESULTS: The cohort included 22,825 veterans, with 83.5% undergoing preoperative UCX (Table 1). Adjusted analysis showed no association between preoperative UCX and postoperative UTI (aOR=0.89; 95%CI [0.72-1.10]; p=0.29) (Table 1). Historically positive UCX (aOR=1.33; 95%CI [1.13-1.57]; p=0.001) was the strongest factor associated with postoperative UTI. Men who had laser enucleation of the prostate (versus TUTP) were less likely to develop postoperative UTI (aOR=0.56; 95%CI [0.31-0.92]; p=0.031). Other patient factors associated with postoperative UTI are detailed in Table 1. Similarly, a historically positive UCX (aOR=1.62; 95%CI [1.51-1.73]; p<0.001) and undergoing laser enucleation (vs. laser vaporization) (aOR=1.83; 95%CI [1.49-2.27]; p<0.001) were associated with higher odds of preoperative UCX testing (Table 2). UTI rates without and with preoperative UCX were 2.8% and 3.1%, respectively (Absolute Risk Reduction=0.3%). Therefore, for every 334 veterans who did not receive a preoperative UCX, one additional veteran would be diagnosed with a postoperative UTI.
CONCLUSIONS: Routine preoperative UCX did not mitigate postoperative UTI risk in endoscopic prostate surgery, suggesting that its use can be guided by the patientís risk profile. Veterans with a historically positive UCX were more likely to receive a preoperative UCX but still had higher postoperative UTI risk. It is still unclear if these patients may be better served by broader spectrum periprocedural antibiotics as opposed to UCX-guided antibiotics.