IntroductionThere are wide-ranging care models to address the triage, evaluation, and disposition of hospitalized patients with urgent Urologic needs. Described here is a novel Acute Care Urology (ACU) service, which aims to provide comprehensive and expeditious inpatient Urologic care. There is limited available data to suggest widespread adoption of a similar model at other institutions or that defines the broad scope of Urologic care which it encompasses. Therefore, we aim to review services provided by an ACU service and highlight the potential value to a busy academic Urologic practice.
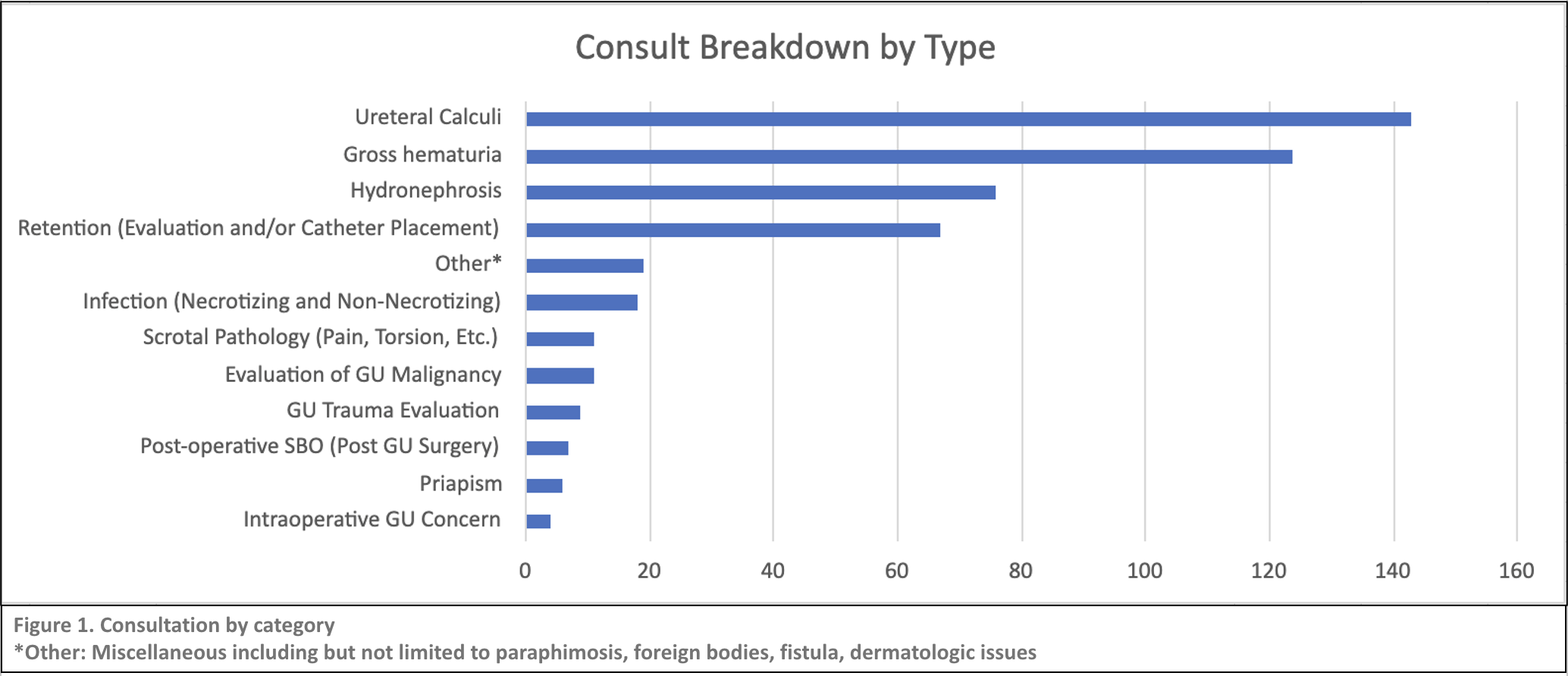
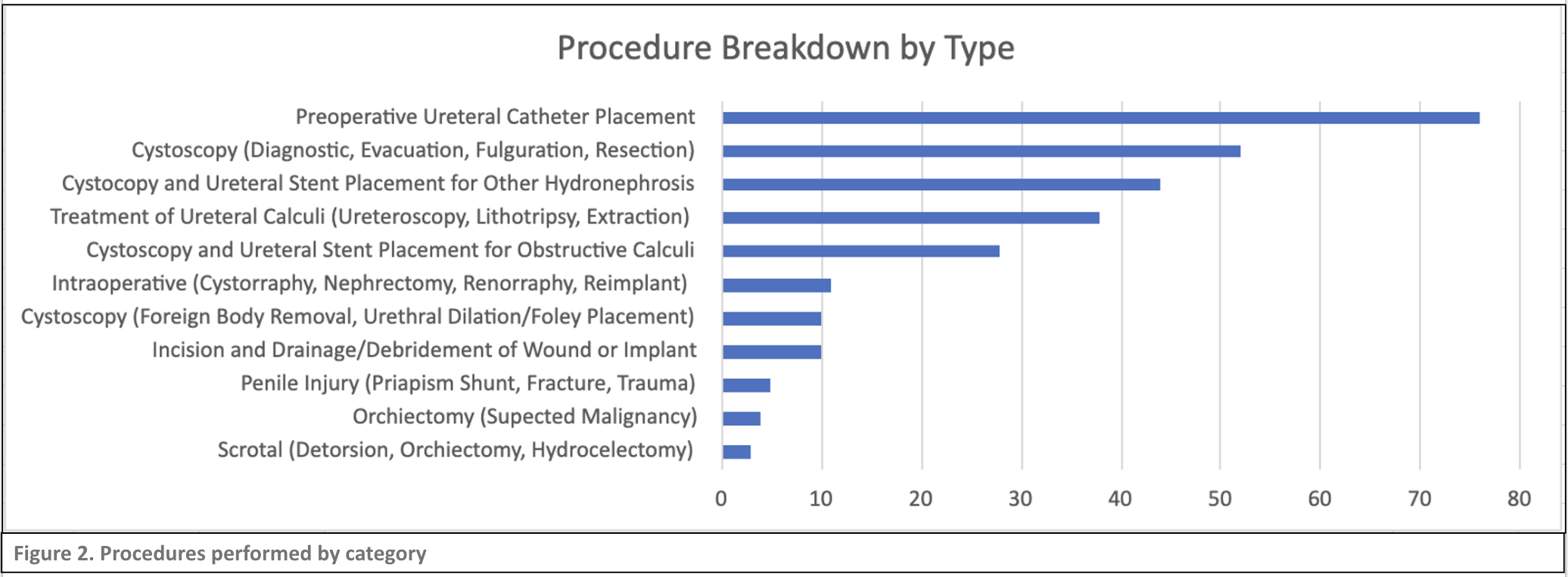
Materials and MethodsAn internal review of the ACU service at the Massachusetts General Hospital between September 2022 to February 2024 was conducted. Inpatient and emergency consultation and operative logs were retrieved from the EMR billing data for two of three ACU surgeons who rotated weekly staffing of the resident driven daytime ACU service and representing roughly half of the total service volume. Each distinct consultation was then further subcategorized based on location and coded diagnosis information as described in Figure 1. Subsequent encounters were excluded. Procedural data was subcategorized based on respective procedural billing codes (Figure 2). Encounters with ambiguous diagnosis/procedural codes were excluded from both cohorts.
ResultsThere were 1060 unique billed encounters that included 767 non-operative consults and 293 procedures performed. 495 of non-operative consults met inclusion criteria, of which 24.8% of visits were completed in the emergency department and 75.2% on inpatient wards. Breakdown of consultation by primary Urologic diagnosis is depicted in Figure 1. 281 of 293 operative procedures were categorized based on billing code. Breakdown and description of procedures performed are shown in Figure 2.
ConclusionsAs anticipated, the most common acute in-hospital Urologic needs are focused on the evaluation and management of hydronephrosis, urinary retention and hematuria. While endoscopic interventions were the most frequently performed procedures, the operative breakdown represents a wide array of genitourinary pathologies. Our analysis highlights both the breadth and depth of Urologic care that can be provided by
a dedicated ACU service. In doing so, the model not only provides patient-facing benefits including greater efficiency and continuity of general Urologic care but also provides further downstream systemic advantages by offloading the burden of inpatient/emergent needs to a centralized service that can then triage and more appropriately refer to Urologic subspecialists. The lack of standardized coding data across all surgeons within the service significantly limited the power and range of this study. This issue has been rectified by a newly implemented ACU-specific billing account, which will allow us to guide future investigations into quality improvement, resource utilization, financial benefits, and replicability from a broader practice standpoint.