Background Radiation cystitis (RC) is a morbid complication of pelvic radiation without guidelines for diagnosis and management. Hyperbaric oxygen (HBO2) therapy has emerged as a non-invasive RC treatment option, however, data regarding its utilization are lacking. The purpose of this study is to evaluate practice patterns in RC diagnosis and management including HBO2 use among Society of Genitourinary Reconstructive Surgeons (GURS) members.
Methods Following Institutional Review Board approval, we administered a web-based survey from January to March 2024 via Research Electronic Data Capture to a purposive group of GURS members managing RC. Respondents were queried on diagnosis and management of RC including HBO2. Survey data were included if core components were completed. Demographic information and barriers to HBO2 utilization were collected. Results were summarized using descriptive statistics.
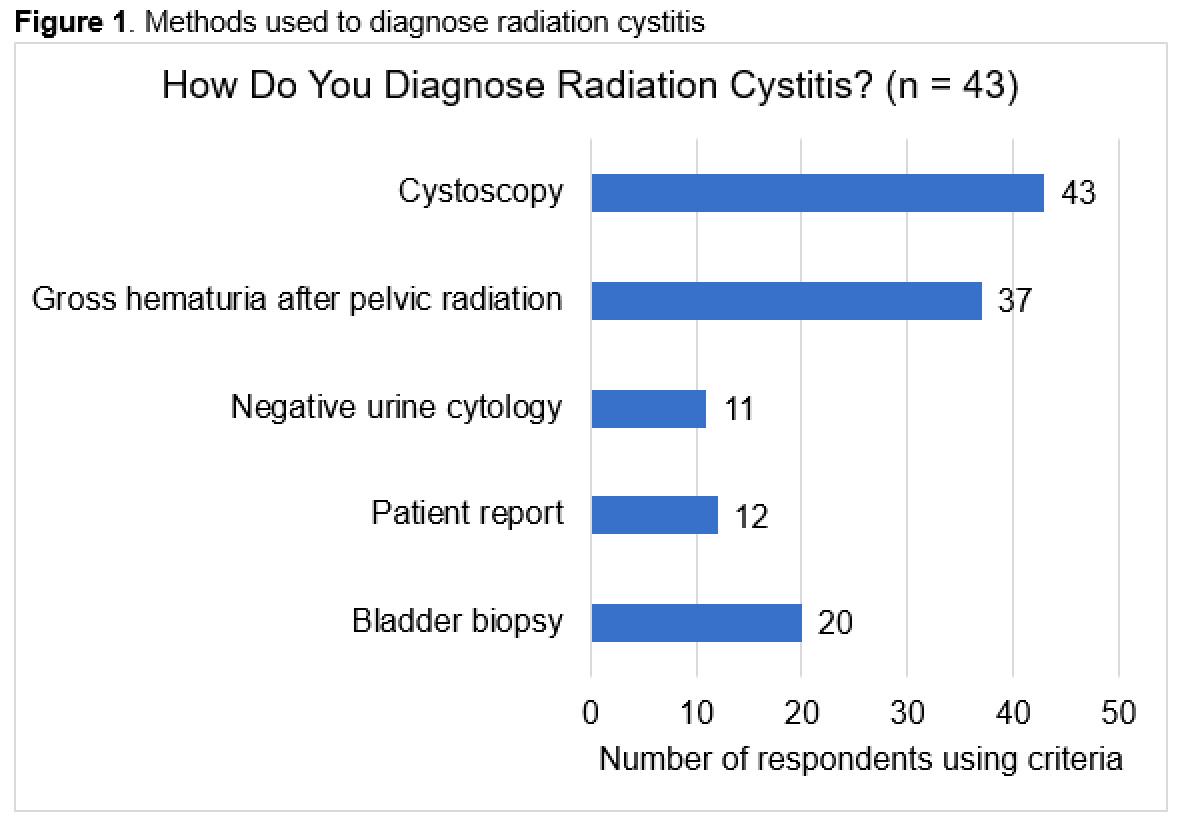
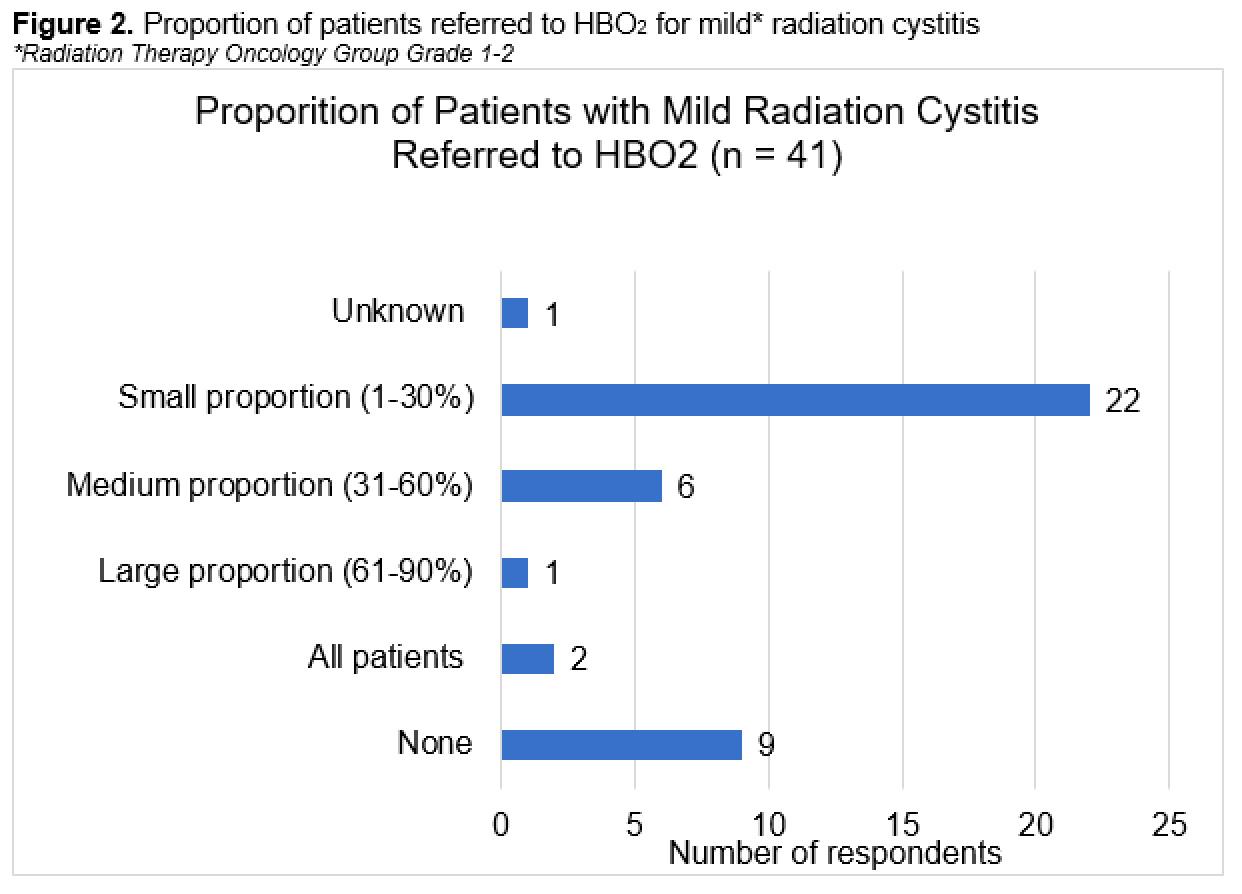
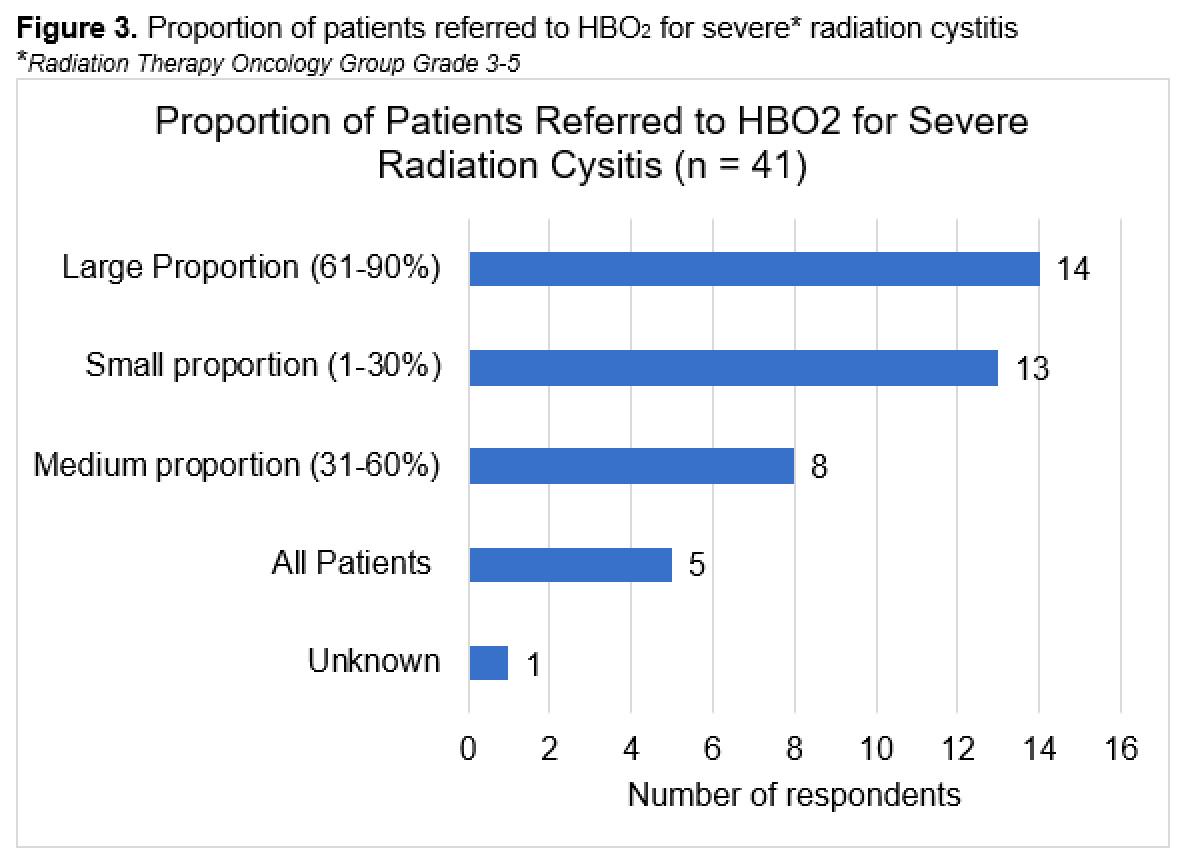
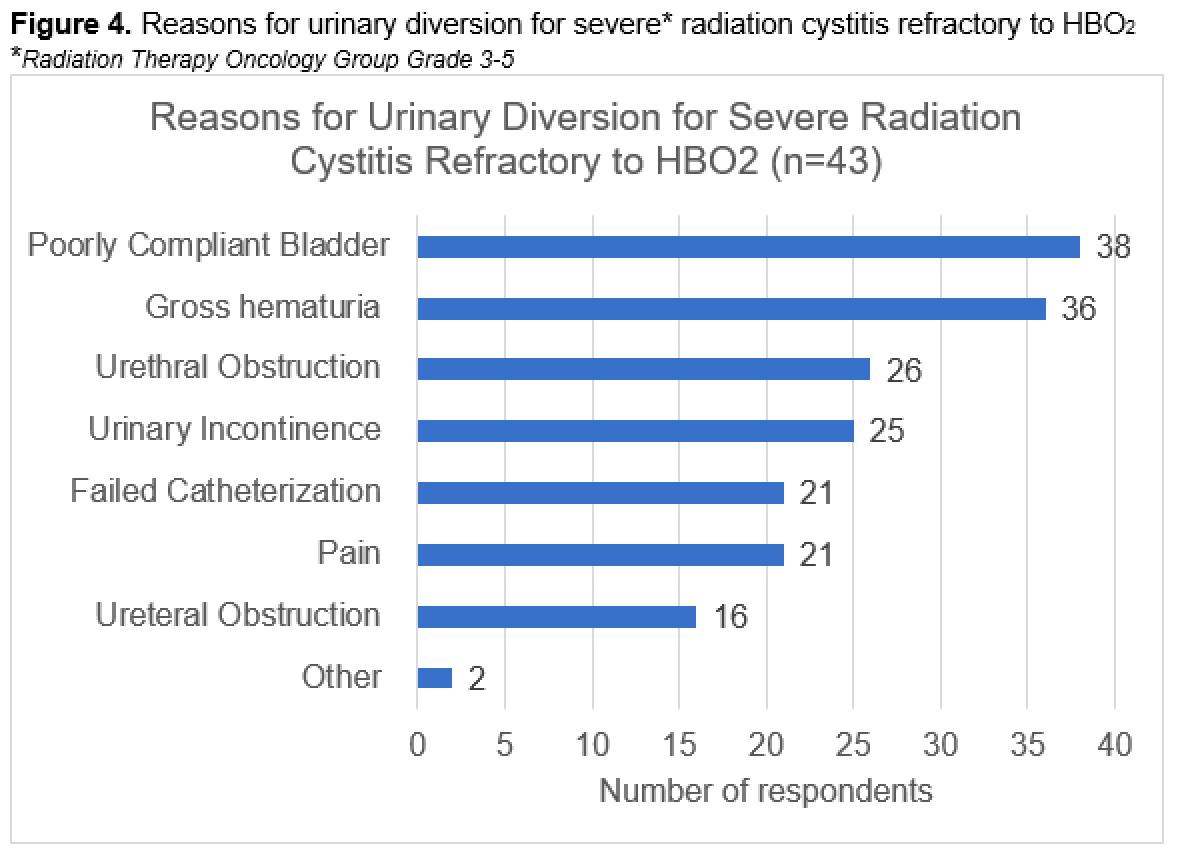
Results A total of 45 participants responded to the survey, mean age 44 (SDą10), practicing 11 years (SDą10), in the USA (39/45), managing at least 1-20 or more RC patients annually. RC diagnostic criteria were variable (Figure 1) with cystoscopy as the most commonly cited diagnostic tool. Only 11/44 respondents used HBO2 monotherapy for initial RC management versus a combination multiple treatments including cystoscopy with fulguration (12/30), bladder embolization (1/30), or bladder instillations (17/30). Most participants ultimately used HBO2 for first or second line treatment (43/44), however with variability in the reported proportions for mild (Figure 2) and severe RC (Figure 3). About half of respondents did not have HBO2 at their institutions and referred patients externally. Reported barriers to HBO2 included number of treatments (30/42), distance (29/42), lack of insurance coverage (27/42), and cost (18/42). A third of respondents noted patients required two or more full HBO2 courses. Surgeons primarily defined HBO2 success by patient report (34/43) and the most frequently listed characteristic associated with HBO2 failure was RC severity (28/43). The majority performed radical cystectomy and urinary diversion for severe RC refractory to two or more HBO2 courses most commonly for poorly compliant, high-pressure bladder (38/43), gross hematuria (36/43), and urethral obstruction (26/43) (Figure 4).
Conclusions In a survey of GURS members, we found wide variation in RC diagnosis and management including HBO2 utilization. Barriers to HBO2 were identified primarily surrounding access and cost. Success was largely defined by patient report. Further research is needed to determine optimum RC diagnostic protocols and management options to develop evidence-based guidelines.