BACKGROUND: Improvements in imaging resolution with micro-ultrasound (microUS) compared to conventional ultrasound (TRUS) may enhance the diagnostic accuracy of image-guided prostate biopsy and may serve as an alternative or supplement to MRI guidance. The objective of this study was to compare Gleason Grade Group (GG) concordance between prostate biopsies performed via TRUS, MRI-TRUS, microUS or MRI-microUS and pathology at radical prostatectomy (RP)
METHODS: We conducted a retrospective study of patients with PCa treated from January 2021 - June 2023 who underwent Robotic assisted RP following TRUS, MRI-TRUS fusion, microUS, or MRI-microUS fusion biopsy in a multi-site single institution study. We compared concordance of GG from biopsy to RP based on highest GG identified in any biopsy core and separately based on systematic or targeted biopsy. We examined clinical and pathologic factors associated with pathologic upgrading using descriptive statistics, univariate and multivariable logistic regression analysis.
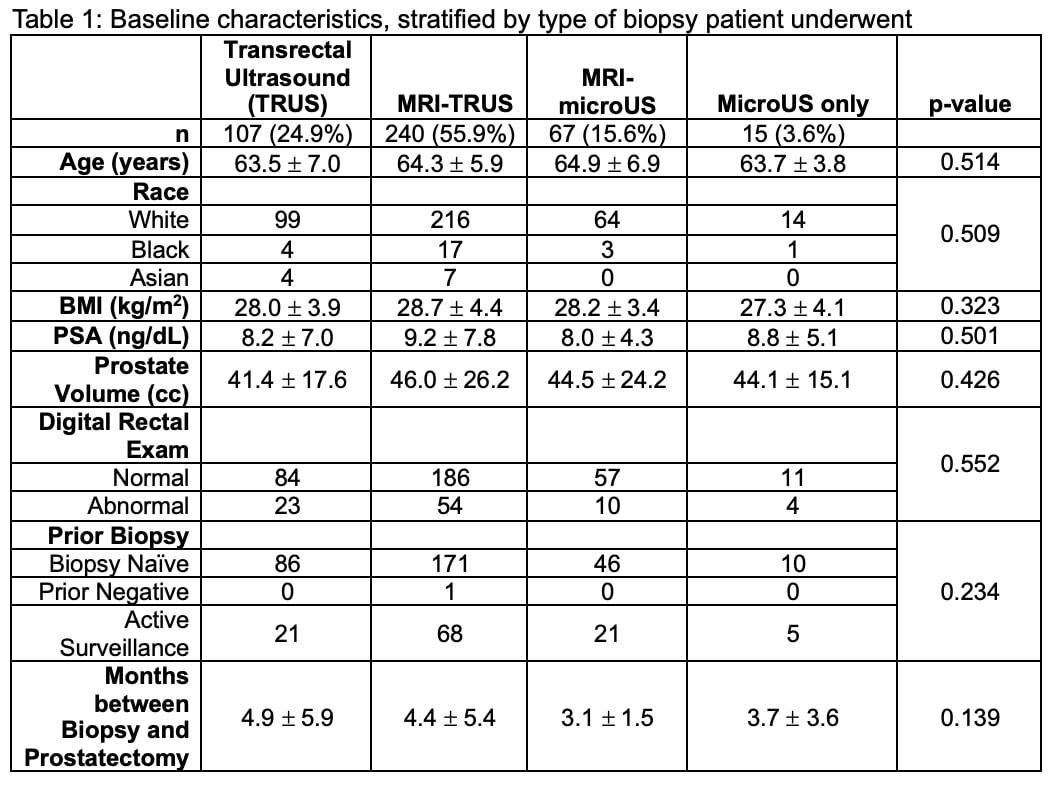
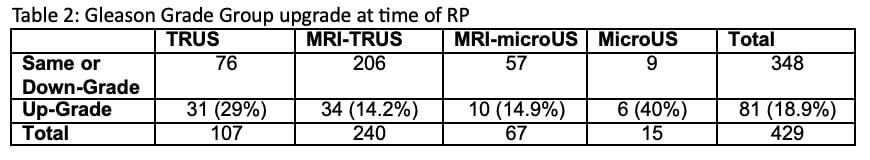
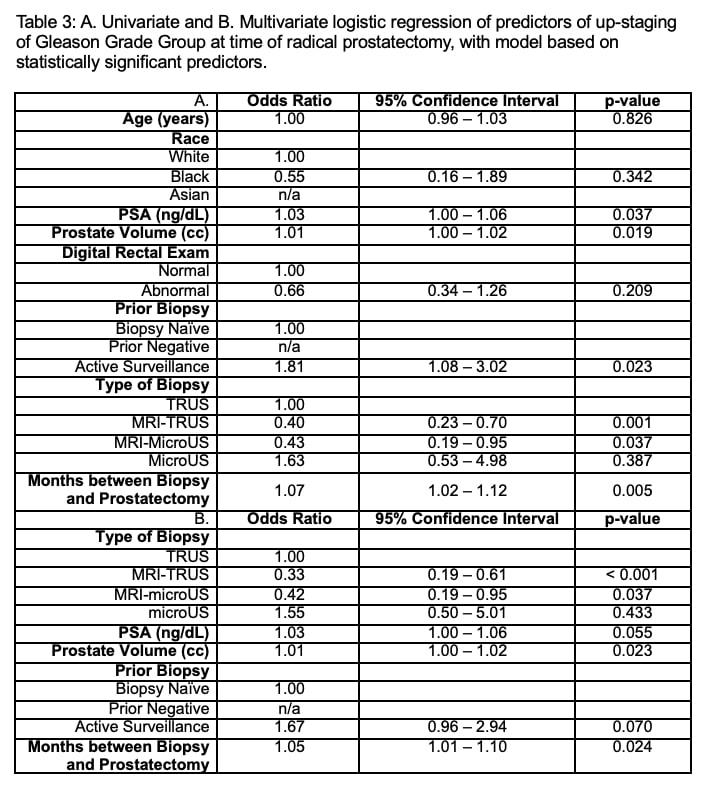
RESULTS: 429 patients were included; 107 (24.9%) had TRUS biopsy performed, 240 (55.9%) MRI-TRUS, 67 (15.6%) MRI-microUS and 15 (3.6%) micoUS alone prior to RP. Patients were similar in terms of age, race, PSA, prostate volume, and prior biopsy status (p>0.05). 81 (18.9%) patients were upgraded on final pathology (TRUS 31 (29%), MRI-TRUS 34 (14.2%), MRI-microUS 10 (14.9%), microUS: 6 (40%)) and 99 were downgraded. 15 (3.5%) of patients experienced a major upgrade (≥2 GG increase). On multivariate analysis both MRI-TRUS (OR: 0.33, 95% CI: 0.19-0.61, p<0.001) and MRI-microUS (OR: 0.42, 95% CI: 0.19 - 0.95, p=0.037) were associated with lower odds pathological upgrading as compared with TRUS biopsy alone. On pairwise comparison there was a significant difference between MRI-microUS and micoUS alone in predicting upgrade (OR: 0.26, 95% CI: 0.08 - 0.90, p=0.034). Pairwise comparisons did not reveal significant differences in odds of grade concordance at RP between TRUS and microUS alone (p>0.05), or between MRI-microUS and MRI-TRUS biopsy (OR: 1.06, 95% CI: 0.49- 2.28 p=0.875). On multivariate, higher prostate volume (OR: 1.01, 95% CI: 0.023, p=0.02) and longer time between biopsy and RALP (OR 1.05, 95% CI: 1.01-1.10, p<0.001) were independent risk factors for upgrading.
CONCLUSIONS:
Both MRI-microUS and MRI-TRUS fusion were associated with improved GG concordance between biopsy and RP pathology compared with TRUS biopsy. We did not identify significant differences between microUS alone and TRUS or between MRI-microUS and MRI-TRUS fusion approaches which may suggest similar benefits in disease sampling.