Abstract Body:
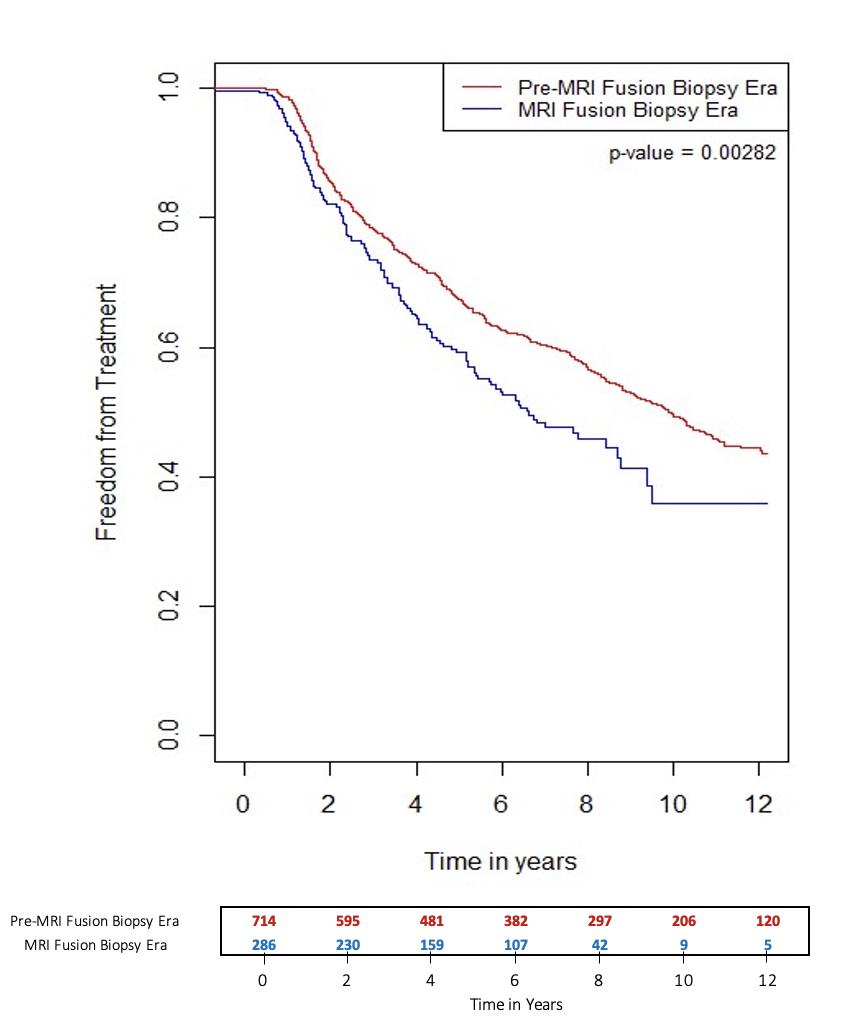
Background:The use of multiparametric MRI (mpMRI) in active surveillance (AS) over the past decade has led to better detection of clinically significant prostate cancer. However, there are limited studies in the literature that investigate the use of mpMRI with AS. Our study aims to compare treatment free survival in the pre-MRI and MRI era at a single institution. Methods:An institutional database of men enrolled in AS between 1996 and 2020 was used with follow-up updated through 2023. The study cohort was divided into pre-MRI and MRI era, defined as patients who underwent a confirmatory biopsy before or after July 2014, when mpMRI and MRI/ultrasound fusion biopsy were included into our AS protocol. A Kaplan-Meier plot was used to analyze the primary outcome, treatment free survival. A multivariable Cox regression analysis was used to control baseline characteristics. Secondary outcomes included adverse pathology on radical prostatectomy specimens, defined as pathologic stage T3 or higher or pathologic node positive disease, and biochemical recurrence (BCR), which were compared using Chi-square tests. All statistical analysis was conducted using R. Results:A total of 1004 patients were included, with 714 men in the pre-MRI era and 290 men in the MRI era. There were no significant differences in PSA (p = 0.27) and Gleason score (p = 0.84) between cohorts. Men in the MRI era were more likely to progress to treatment with a shorter median time to treatment (6.7 versus 4.4 years, p = 0.003) (Figure 1). Analysis of adverse pathology demonstrated no significant difference (17.4% in pre-MRI versus 15.5% in MRI era, p = 0.89). Analysis of BCR demonstrated a statistically significant lower rate of BCR in the MRI era (14.8% in pre-MRI versus 4.8% in MRI era, p = 0.006). Median follow-up time was 9.9 years (6.6-12.5 years) in the pre-MRI era and 6.8 years (4.6-8.0 years) in the MRI era. Conclusion:The use of mpMRI and MRI/ultrasound fusion biopsy in AS results in earlier time to treatment and patients continue to crossover from AS to treatment with longer follow-up times. While our data demonstrates a statistically significant lower risk of BCR in men from the MRI era who were treated, further follow-up time is needed to better evaluate this.