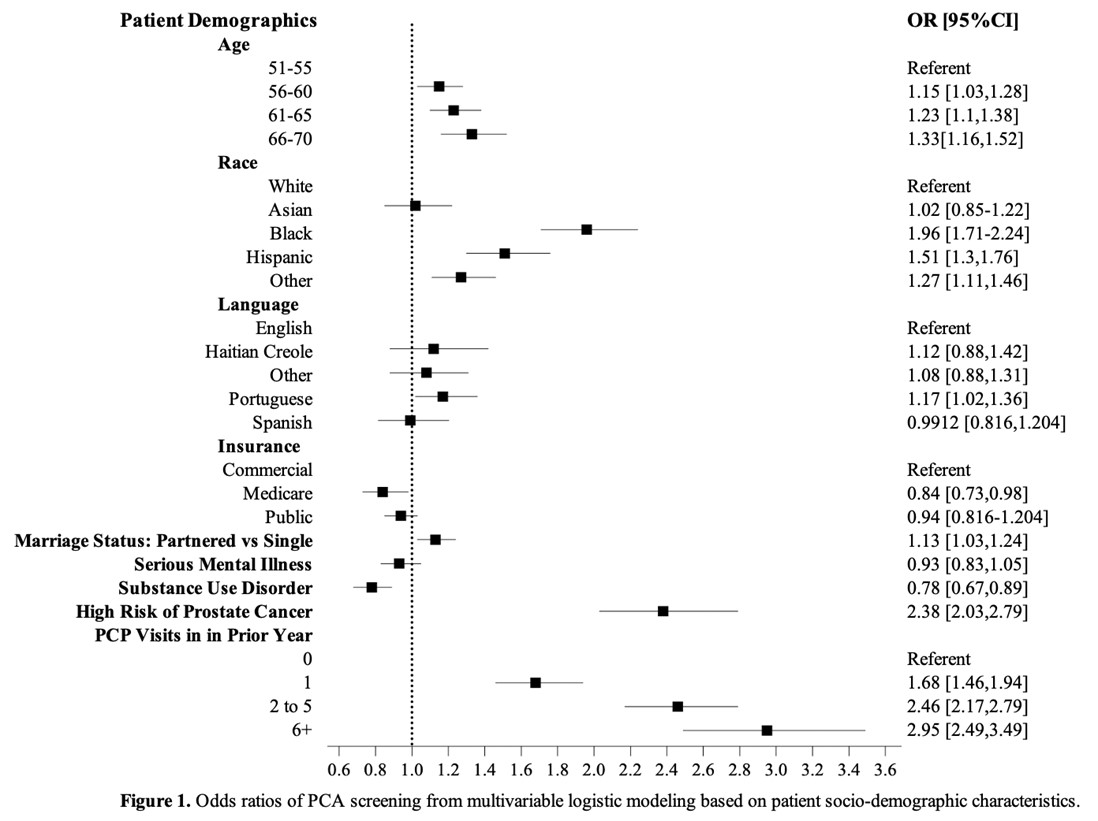
Background: Health safety-net (HSN) populations are comprised of diverse vulnerable groups, each facing unique and complex barriers to prostate cancer screening (PCS). Existing literature underscores racial disparities in PCS, with notably lower PCS rates among Black, Hispanic, and Asian men compared to White men. Less is known regarding PCS disparities within individual ethnic groups. Additionally, lower PCS rates are reported among men with limited English proficiency (LEP) and those with substance use disorder (SUD). This study evaluates whether traditional PCS disparities persist within a HSN healthcare system tailored to support underserved populations through supported access to insurance, Primary Care Providers (PCP), and interpreters. Furthermore, it seeks to elucidate new opportunities for targeted PCS interventions within this vulnerable population.Methods: A retrospective cohort study using electronic health record data was conducted at an urban safety-net hospital. Male patients aged 51-70 years with a PCP visit from 2018-2019 were included. The primary outcome was PSA screening, defined as receiving a PSA blood test within two-years prior to the PCP visit. Investigated patient characteristics included self-reported race and ethnicity, language, insurance, marriage status, median household income, serious mental illness (SMI), SUD, and family history of prostate cancer (PCa). Bivariate analyses using chi-squared tests and multivariable logistic regression analyses were performed to compare PCS rates between groups.Results: Of 10,059 patients, 40.4% had PCS. More than half of the study population was of non-White race (57.3%) and non-North American/European ethnicity (61.4%). 31.2% of the population had LEP, 17.8% had SMI, and 13.2% had SUD. All patients in the study population had insurance. The PCS rate was significantly lower among White compared to Black (34.9%, 95%CI 0.33-0.36 vs. 51.6%, 95%CI 0.49-0.54, p<0.001) and Hispanic patients (34.9%, 95%CI 0.33-0.36 vs. 44.5%, 95%CI 0.42-0.47 p<0.001). English-speaking patients had a lower screening rate (38.9%) than any other language. In multivariable analysis, patients of White race had significantly lower odds of PCS compared to Black patients (OR 1.96, 95%CI 1.71-2.24, p<0.001) and Hispanic patients (OR 1.51, 95%CI 1.3-1.76, p<0.001). Patients of North American/European ethnicity had significantly lower odds of PCS compared to all other ethnicities (ORs: 1.29-2.28), except for patients who identified as Asian and “Other” ethnicities. English-speaking patients had significantly lower odds of PCS than Portuguese-speaking patients (OR 1.17, 95%CI 1.02-1.36, p=0.028). Patients diagnosed with SMI and patients with SUD had lower odds of undergoing screening compared to their counterparts, with statistically significant results observed for patients with SUD (OR 0.78, 95%CI 0.67-0.89, p = <0.001). Conclusions: Within a HSN system designed and implemented to meet the needs of underserved populations, the traditional racial and sociodemographic disparities in PCS were not evident.