BACKGROUND: Many patients with prostate cancer have an indolent form of disease that can be safely managed with active surveillance (AS). However, accurate and dynamic risk assessment of disease progression is critical to performing safe AS. Conditional survival analysis accounts for how the probability of disease progression dynamically changes over time. Time-Varying analysis accounts for covariates which change during a follow-up period. We aimed to study the conditional survival of patients managed with AS, and examine the time-varying covariate of multiparametric magnetic resonance imaging (mpMRI) performed during the AS period.
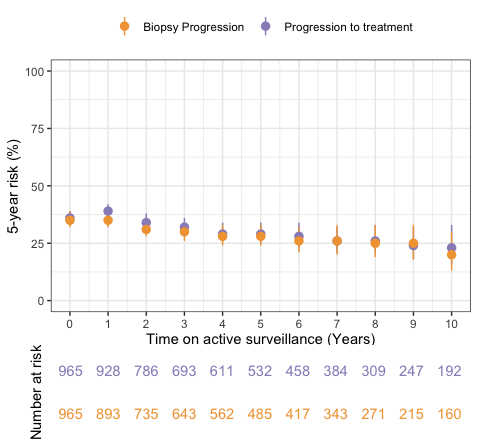
METHODS: We retrospectively reviewed our institutional database of patients with localized prostate cancer enrolled in AS from 1996 to 2018 with follow-up through 2023. Our AS protocol includes prostate-specific antigen and digital rectal exam every 6 months for 3 years, then annually when clinically indicated. Mandatory confirmatory biopsy is done at 12-18 months. mpMRI and additional surveillance biopsies are done at the discretion of physician and patient. Patients were included in this analysis if on initial biopsy they had grade group 1-2 disease, up to 50% of cores positive, and up to 50% maximum core involvement. Primary outcome measures were biopsy progression-free survival and treatment-free survival. Standard static Kaplan-Meier analysis was performed, and then five-year conditional survival estimates were derived for both outcomes. Finally, a Cox regression model was performed with several standard clinical factors and the Prostate Imaging Reporting & Data System (PIRADS) score on mpMRI treated as a time-varying covariate.RESULTS: 965 patients were included in this analysis cohort. Median follow-up time was 8.0 years (IQR 5.8 - 11.0). At diagnosis, the overall 5-year risk of biopsy progression and progression to treatment was 35% (95% CI 32-39%) and 36% (95% CI 33-39%), respectively. The 5-year risk decreased over time for patients who survived additional years on AS (Figure). After 5 years on AS, the 5-year risk of biopsy progression and progression to treatment was 28% (95% CI 24-33%) and 29% (95% CI 25-34%), respectively. 647 patients had a mpMRI performed during the AS period. Time-varying analysis demonstrated that patients with mpMRI showing a PIRADS 3 (HR 3.93, 95% CI 2.47-6.26, p < 0.001), PIRADS 4 (HR 5.52, 95% CI 3.91-7.80, p < 0.001), or PIRADS 5 (HR 9.89, 95% CI 6.56-14.9, p < 0.001) lesion were independently associated with having biopsy progression on AS compared to patients with lower grade lesions.
CONCLUSIONS: We found that the probability of biopsy progression and progression to treatment decrease over time among patients who remain on AS longer. In addition, patients with a mpMRI obtained during AS demonstrating a PIRADS 3 or greater lesion have a significantly increased association with biopsy progression. Future directions include creating a prospective dynamic risk calculator for patients on AS that incorporates time survived on AS and other contemporary clinical factors including mpMRI.