Background:
Prostate Imaging Reporting & Data System (PI-RADS)3 lesions pose a clinical management challenge due to their MRI characteristics, which often exhibit significant overlap with benign conditions, particularly in transition zone vs peripheral zone lesions (TZ, PZ). We investigated the association between isolated PIRADS3 lesions of the TZ vs PZ and the incidence of clinically significant prostate cancer (csPCa) on systematic and targeted prostate biopsy (SB, TB).
Methods:
We retrospectively reviewed an institutional database of patients who underwent 3-Testla mpMRI-fusion followed by targeted and systematic transrectal biopsy (TB, SB) at a tertiary care center between 2016-2021. We compared incidence of csPCa (Gleason Grade Group 2 or higher) in patients with solitary TZ-only PIRADS-3 and PZ-only PIRADS-3 on SB and TB. Patients with PIRADS 4-5 and/or lesions in both TZ and PZ were excluded, in addition patients with history of prostate cancer where excluded. T-test and Fisher exact test were done using R 4.3 (R Core Team, 2023).
Results:
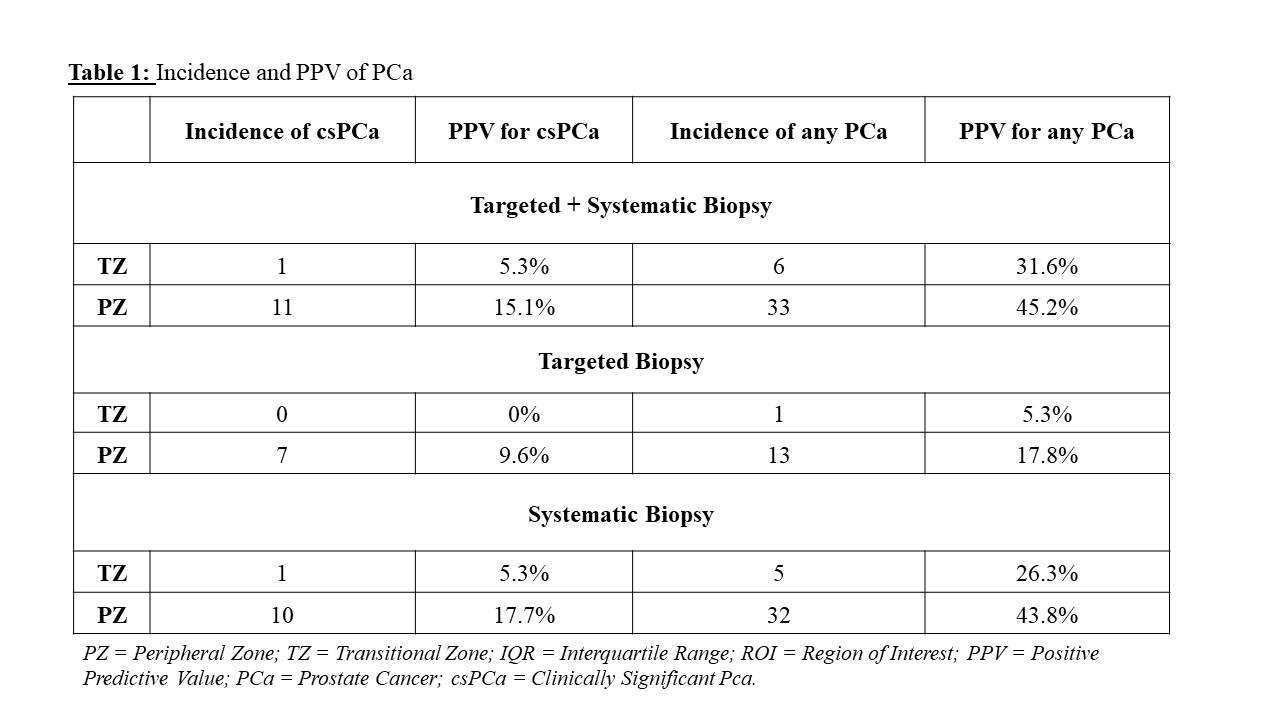
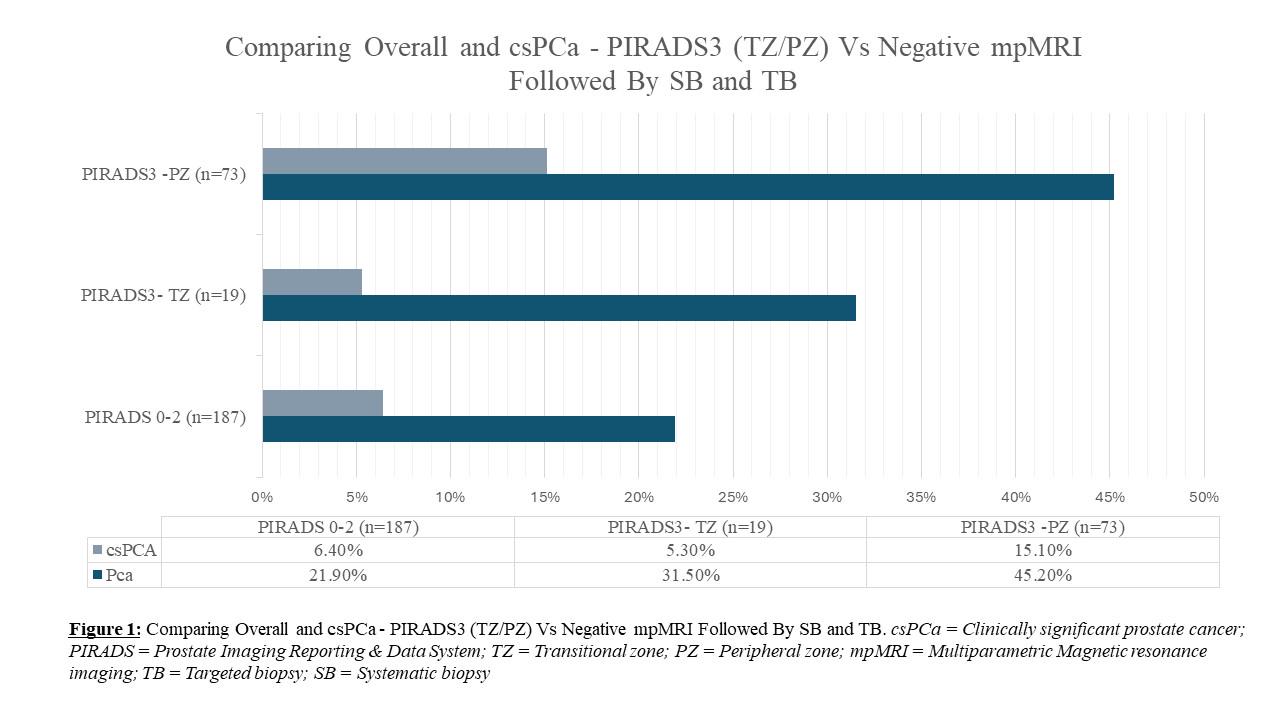
Of 1913 patients, we identified 110with PZ-only and 38 with TZ-only PIRADS-3 lesions. 73 patients in PZ-only and 19 in TZ-only met inclusion criteria. No statistically significant difference was noted between the PZ and TZ groups in terms of age (63 vs 67 , p = 0.35), median PSA (6.2ng/ml vs 8.15ng/ml; p = 0.11), prostate size (53ml vs 69ml, p = 0.3), median PSA density (0.1 [IQR 0.05] vs 0.9 [0.11])ng/ml2, average number of PIRADS3 lesions (1.2±0.6 vs 1.05±0.2, p = 0.12), or median number of targeted cores obtained (3 [IQR 0.25] vs. 3 [IQR 0], p = 0.78) in patients who underwent TB. On SB, the incidence of csPCA was higher in patients with PZ rather than TZ PIRADS-3 lesions (10/73 vs 1/19, p = 0.28). Similarly, csPCA was more common in TB of PZ vs TZ PIRADS 3 lesions (7/73 vs 0/19, p = 0.33). Compiling above results, the positive predictive values of PIRADS3 as a marker of csPCA was 5.3% and 0% for TZ lesions on SB vs TB, respectively, compared to 17.7% and 9.6% in the PZ (Table 1). Figure 1 illustrates the rates of diagnosis of PCa and csPCa on TB+SB when PIRADS 3 is found in PZ and TZ, in comparison to negative (PIRADS<3) mpMRI results.
Conclusions:
PIRADS3 lesions are rarely associated with csPCA on systematic and targeted biopsy, particularly when in the TZ, an important factor when considering biopsy in patients with isolated TZ lesions.