Background:Ureteroscopy (URS) ranks as the number one procedure newly graduated urology residents express confidence in performing independently. Research indicates that continued proficiency and maintenance of skills results from ongoing, high-volume, frequent procedural experience. We sought to evaluate the URS case experience through post-graduate years (PGY) of residency training and self-reported confidence in this procedure.
Methods:A 5-point Likert-score questionnaire assessing overall trainee confidence performing URS and confidence in six individual procedural steps (cystoscopy/ureteral cannulation/retrograde pyelogram, ureteral access sheath placement, flexible ureteroscopy, laser setup/laser lithotripsy, fragment retrieval/basketing, stent decision-making/placement) was completed by current PGY2 - PGY5 residents at three academic training programs in New England. Corresponding number of URS cases performed was determined by review of Accreditation Council for Graduate Medical Education (ACGME) case logs recording ICD-10 CPT codes for URS and stratified by training year. Incomplete surveys and/or case logs were excluded from analysis. Descriptive statistics were summarized for continuous variables.
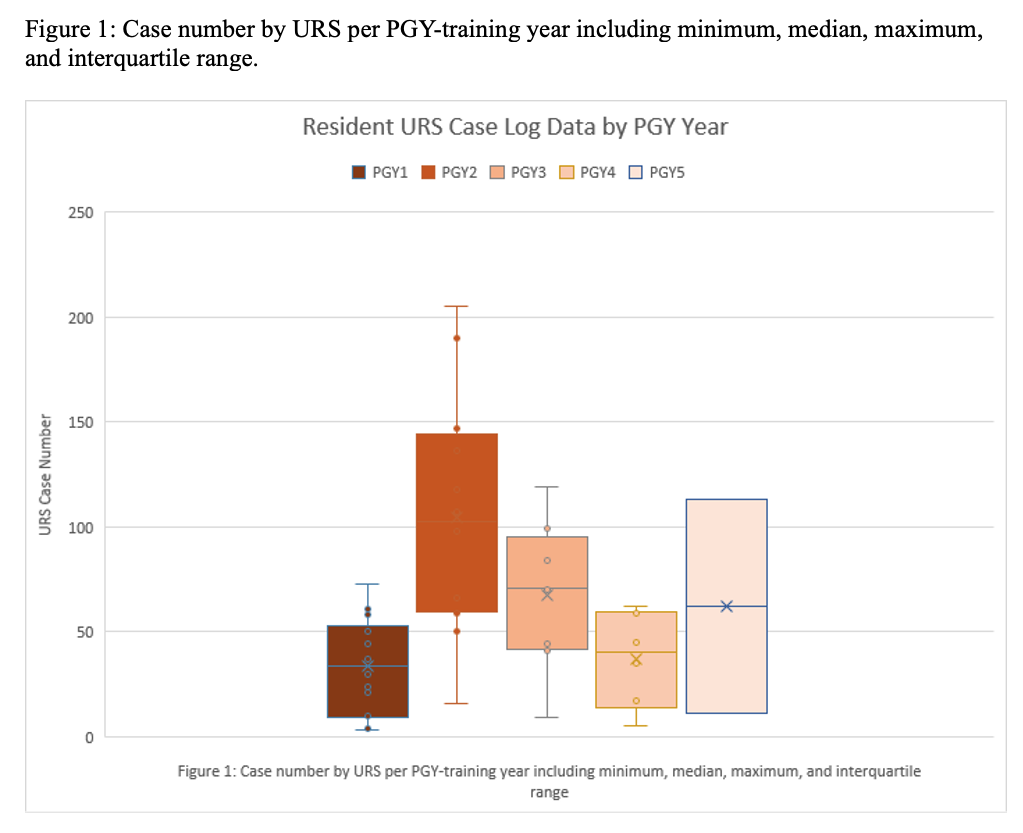
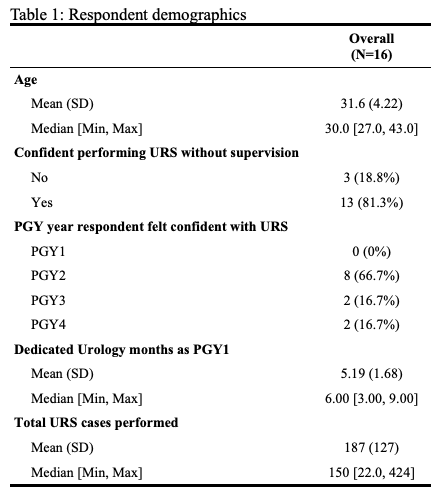
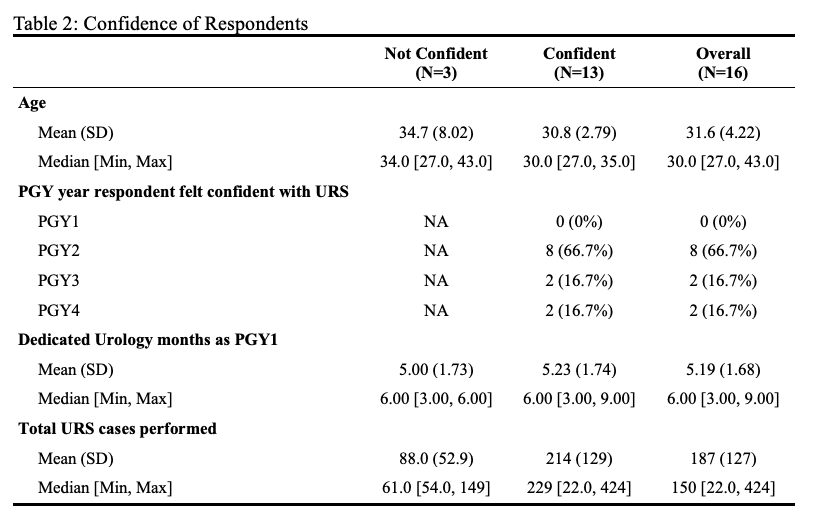
Results:Twenty-three residents in three New England AUA residencies responded. 16 met inclusion criteria (Table 1). 13/16 (81%) of residents felt capable of performing ureteroscopy with laser lithotripsy unsupervised with the majority gaining that confidence during PGY2 (66.7%). The three residents who reported lack of confidence in unsupervised URS were PGY2 in training. Procedural confidence in stent decision-making and placement was highest (75.0% self-rated as “resident expert, ready for practice”). Ureteral access sheath placement and laser setup/laser lithotripsy were rated least confident, requiring passive attending assistance during PGY2 year only. No PGY3 - PGY5 residents reported requiring passive attending assistance in any of the six procedural steps queried (Table 2). The highest URS case volume was seen during PGY2, with a decline thereafter (Figure 1).
Conclusions:Confidence in performing URS occurs early in training, coinciding with high endoscopic case volume and repetition during PGY2. Sustained confidence is observed in senior resident years despite a decline in URS case volume and procedural frequency as residents work on developing other surgical skills. Previously published studies suggest that sustained repetition is key to mastery. Reduced exposure to URS cases in senior training years may have implications for patient outcomes and readiness for independent practice after graduation. Further investigation is warranted to determine optimal case frequency for the maintenance of proficiency and better methodology for evaluating skill progression and providing feedback.