Early Survival Outcomes after Neoadjuvant Chemotherapy for Muscle Invasive Bladder Cancer
Joshua A. Linscott, MD, PhD, Randie E. White, MD, Stephen T. Ryan, MD, Moritz H. Hansen, MD, Matthew H. Hayn, MD, Jesse D. Sammon, DO.
Maine Medical Center, Portland, ME, USA.
BACKGROUND: Neoadjuvant chemotherapy (NAC) should be offered to eligible patients with non-metastatic muscle invasive bladder cancer (MIBC) prior radical cystectomy (RC). Multiple studies have demonstrated an overall survival benefit when neoadjuvant chemotherapy is used, although the absolute survival benefit is relatively modest. Our academic center provides most cystectomy care in a rural state and approximately two thirds of patients receive a full treatment course of NAC prior to cystectomy. We sought to examine our early overall survival outcomes based on receipt of NAC.
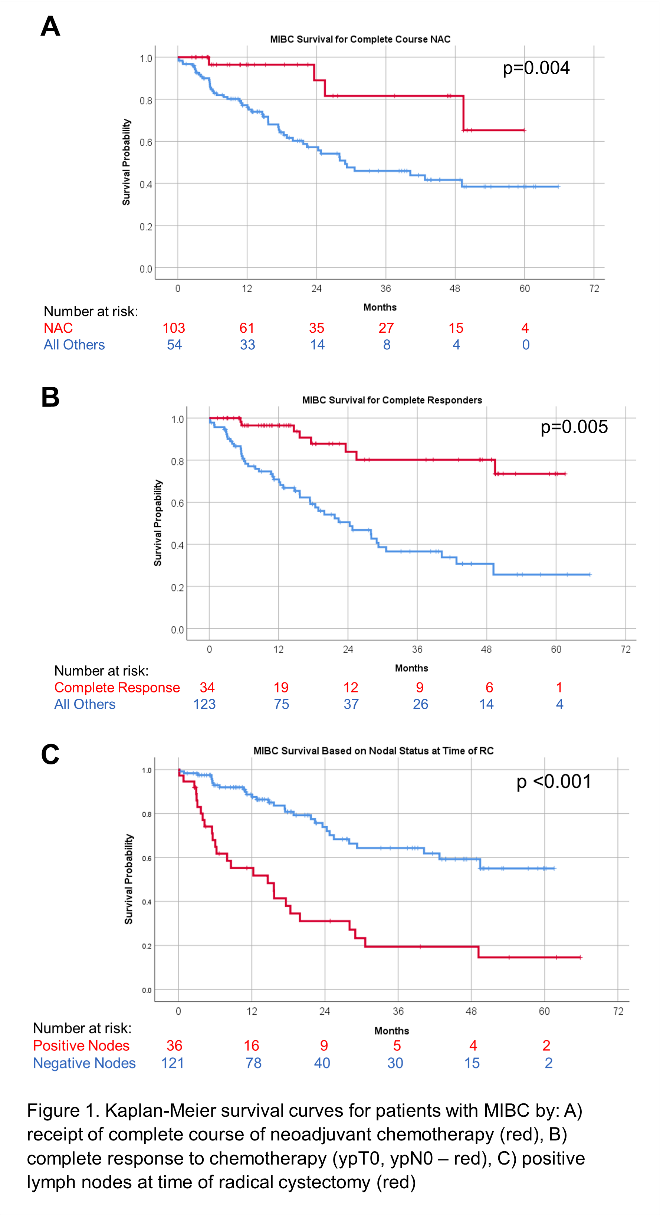
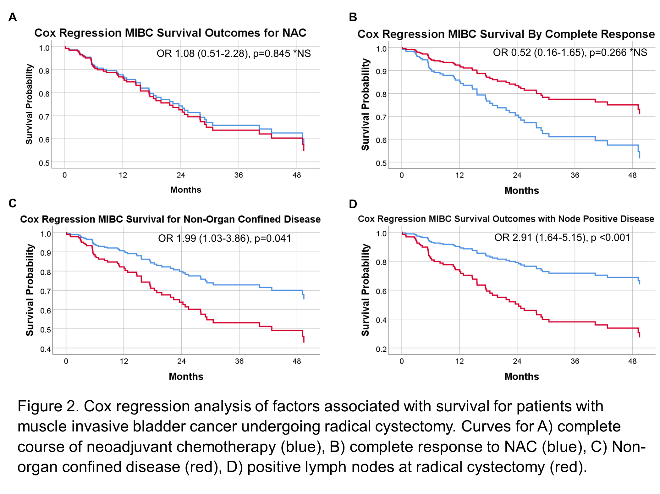
METHODS: Patients with MIBC who underwent RC from 2015-2021 in our database were identified. Demographics, treatment variables, surgical pathology, length of follow up, and vital status were recorded. Kaplan-Meier and Cox Regression controlling for sex, age, Charleston comorbidity index, organ confined disease, and nodal status were performed in SPSS.RESULTS: 158 patients with MIBC underwent cystectomy from 2015-2021. 65.8% (104/158) received a full course of NAC with most having cisplatin-based therapy (95.1%). Younger patients were more likely to receive NAC and <20% of octogenarians received NAC (P<0.001). Complete response rate was 32.7%. Median overall survival for MIBC patients improved with a NAC to 45.4 months (95%CI 39.3-51.5) versus 28.0 months (95%CI 21.7-34.3, p=0.004, figure 1). Those with complete response (CR) to NAC had an OS of 52.0 months (95%CI 43.3-58.7) compared to 36.4 months (95%CI 30.9-41.9, p=0.005) if not receiving NAC or without complete response. For all MIBC patients, positive lymph nodes (+LNs) were associated with worse overall median survival of 21.3 months (95%CI 13.5-29.1) versus 44 months (95%CI 39.0-49.1, p<0.001). Median follow up for the cohort was 15.0 months [IQR 7.5-29.0]. Overall, NAC did not improve survival when controlling for other factors by Cox Regression analysis. CR appeared to improve prognosis but was not statistically significant and limited by a limited number of the cohort reaching the survival end point. Non-organ confined disease [OR 1.99 (1.03-3.86), p=0.041] and +LNs [OR 2.91 (1.64-5.15), p<0.001] were the most significant factors and associated with worse outcomes regardless of NAC receipt (figure 2)
CONCLUSIONS: We found improved survival for MIBC with NAC prior to RC, but this benefit is not maintained when controlling for other factors and likely reflects a selection bias of healthier patients being more likely to receive NAC. CR, and locally advanced or +LNs at time of surgery are more likely to predict survival outcomes. Factors predicting response to NAC (i.e. genetic/genomic markers) are needed to guide who may benefit from NAC.
Back to 2022 Abstracts


