Robotic Versus Open Radical Cystectomy for Urothelial Carcinoma of the Bladder
Joseph B. Black, MD, PHD1, Sumedh Kaul, MS1, Aaron Fleishman, MPH1, Ruslan Korets, MD1, Peter Chang, MD, MPH1, Andrew Wagner, MD1, Simon Kim, MD2, Joaquim Bellmunt, MD, PHD1, Irving Kaplan, MD1, Aria F. Olumi, MD1, Boris Gershman, MD1.
1Beth Israel Deaconess Medical Center, Boston, MA, USA, 2University of Colorado Anschutz Medical Center, Aurora, CO, USA.
BACKGROUND: The comparative effectiveness of robotic-assisted (RARC) versus open radical cystectomy (ORC) in the management of urothelial carcinoma of the bladder (UCB) remains uncertain. Limited randomized trial evidence suggests similar perioperative outcomes and 2-year progression-free survival, but long-term survival outcomes and real-world data are lacking. We therefore evaluated the comparative effectiveness of RARC and ORC using a nationwide oncology dataset.
METHODS: We conducted observational analyses designed to emulate the completed RAZOR trial using the NCDB. Specifically, we identified adults age 37-89 years with Charlson 0-1 diagnosed with cT1-4 cN0-1 cM0 UCB from 2010-2015 and treated with RARC or ORC with LND at a hospital performing an average of >10 RCs per year. We then examined the associations of surgical approach with perioperative outcomes and overall survival (OS) using propensity score methods with stabilized inverse probability of treatment weights (sIPW), with Cox models further adjusted for imbalanced pathologic features (pT and pN stage).
RESULTS: A total of 3,493 patients were included in the cohort, of whom 2,492 (71%) underwent ORC and 1,001 (29%) underwent RARC. Median follow-up was 29.5 months. After sIPW reweighting, pre-treatment baseline characteristics were well-balanced. After adjustment, RARC was associated with a statistically significant but clinically insignificant higher lymph node (LN) yield (median 20 vs 18 LNs; p<0.01) and shorter length of hospitalization (median 7 [IQR 5-8] vs 7 [IQR 6-10]; p<0.01), but there were no differences in positive surgical margins (8% vs 8%; p=0.64) or 30-day readmissions (10% vs 9%; p=0.80). After adjustment, there was no difference in OS between RARC and ORC (Figure 1; 5-year OS 57% vs 55%; p=0.28; HR 0.93, 95%CI 0.80-1.07). OS treatment effects were similar when examined across cT stage, cN stage, and age.
CONCLUSIONS: In observational analyses designed to emulate the completed RAZOR trial, RARC was not associated with statistically significant differences in positive surgical margins, 30-day readmissions, or OS compared to ORC. 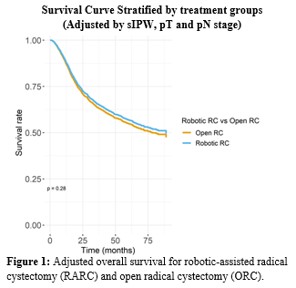
Back to 2022 Abstracts


