Outpatient Single Port Robotic Radical Prostatectomy: Outcomes of 157 patients and Analysis of Learning Curve
Juliana E. Kim, AB1, Isaac E. Kim, Jr., ScB2, Saum Ghodoussipour, MD3, Moses M. Kim, MD, PhD4, Isaac Yi Kim, MD, PhD, MBA5.
1Section of Urologic Oncology, Rutgers Cancer Institute of New Jersey and Division of Urology, Rutgers Robert Wood Johnson Medical School, Rutgers, The State of New Jersey, New Brunswick, NJ, USA, 2Alpert Medical School of Brown University, Providence, RI, USA, 3Section of Urologic Oncology, Rutgers Cancer Institute of New Jersey and Division of Urology, Rutgers Robert Wood Johnson Medical School, Rutgers, The State of New Jersey, New Brunswick, NB, USA, 4Orange County Urology Associates, Irvine, CA, USA, 5Department of Urology, Yale School of Medicine, New Haven, CT, USA.
Background: Robot-assisted radical prostatectomy (RARP) has been a standard of care in the management of prostate cancer since the early 2000's. With four articulated instruments, RARP greatly reduced postoperative recovery times and blood loss compared to open prostatectomy. In 2018, the USFDA approved the da Vinci single-port (SP) system, in which four instruments are still utilized, but enter via a single-site access trocar. Herein, we report the largest case series for SP-RARP to date. Our primary aim is to analyze the peri-operative and short-term outcomes of this procedure. Our secondary aim is an assessment of the learning curve with this new platform.
Methods: A total of 157 patients underwent SP-RARP by two surgeons who have completed over 3000 multiport robotic surgeries. For one surgeon, the first seven cases were done via a transperitoneal approach. The remaining cases used a preperitoneal approach. IRB-approved prospectively collected data was used. Basic demographic pre-operative variables and peri-operative outcomes were analyzed.
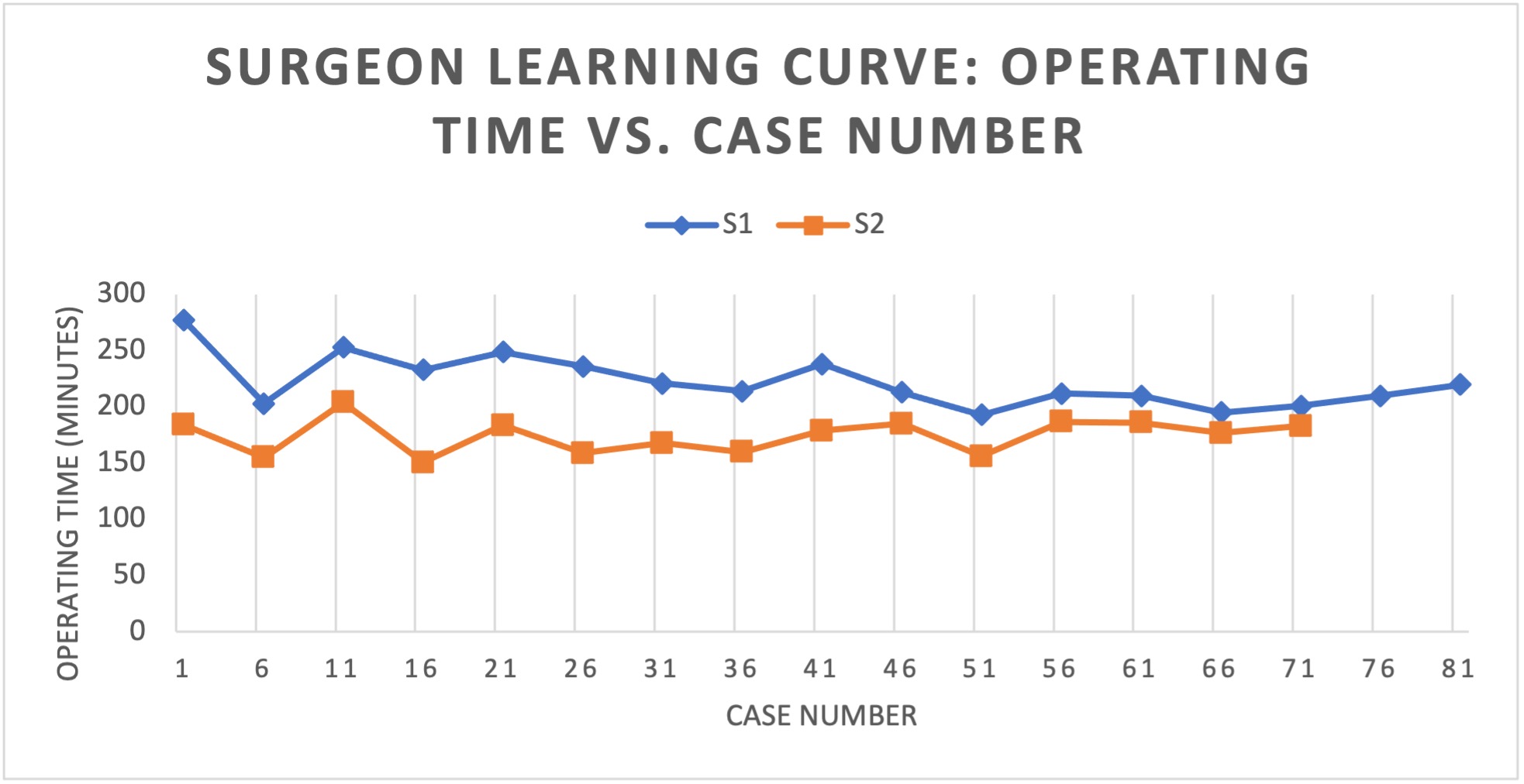
Results: Median patient age and PSA were 63 years and 6.3 ng/mL prior to treatment (IQR 4.7 - 8.2 ng/mL). Average prostate weight was 47 g. The median operating time was 195 min (IQR 165 - 221.25 min) with a median EBL of 100 mL (IQR 100 - 200 mL). The operating times of each surgeon are shown in Figure 1. Surgeon 1 stabilized their operating time around case #56, and Surgeon 2 stabilized around case #26 (Figure 1). Surgeon 2 used the transperitoneal approach for the first seven cases. There were no intraoperative complications. There were six total post-operative complications (3.8%) and four (2.5%) were high grade according to the Clavien-Dindo scale for surgical complications (IIIa or higher). The overall positive margin rate was 28% (26%, 36%, and 40% for T2, T3a, and T3b tumors respectively). 110 patients went home same day, 45 stayed one night at the hospital, with only two patients requiring to stay in the hospital for more than one night (70%, 29% and 1% respectively).
Conclusions: This case series analysis confirms the safety and efficacy of SP RARP with acceptable short-term outcomes. There is a significant learning curve for this new modality due to reduced flexibility of the instruments and diminished surgical field. The initial learning curve may be shortened by using the transperitoneal approach. Same day discharge appears to be an early benefit of the SP platform.
Back to 2022 Abstracts


