Safety and Pathologic Findings of Robotically Assisted Super-Extended Pelvic Lymph Node Dissection for Prostate Cancer
Ryan Daigle, BS, Tara McLaughlin, PhD, Ilene Staff, PhD, Joseph Tortora, MS, Akshay Gangakhedkar, BS, Joseph Wagner, MD.
Hartford Hospital, Hartford, CT, USA.
BACKGROUND: The extent of pelvic lymph node dissection for prostate cancer varies greatly between surgeons and centers, and the therapeutic benefit remains to be determined. Here we examine the safety and pathologic findings when performing a super-extended pelvic lymph node dissection for high risk prostate cancer and we compare these outcomes to patients who underwent extended pelvic lymph node dissection. METHODS: We retrospectively queried an IRB approved prospectively maintained database to identify cases of robotic assisted radical prostatectomy (RARP) with lymph node dissection performed by a single surgeon between May 2016 and September 2021. An extended pelvic lymph node dissection (ELND) included external iliac, internal iliac, and obturator lymph nodes. Patients with NCCN high/very high and higher unfavorably intermediate (eg high volume Grade Group 3 with PSA approaching 20) risk prostate cancer patients were offered a super-extended pelvic lymph node dissection (sELND) which also included the common iliac, aortic bifurcation, and pre-sacral lymph nodes. We compare ELND and sELND with regards to perioperative parameters, length of stay, complications, and pathologic findings. RESULTS: 733 patients had RARP with lymph node dissection. 572 patients underwent ELND and 161 patients underwent sELND (Table 1). Robot time was longer for the sELND group (p<.001). As sELND was offered to higher risk patients, the number of salvage prostatectomies, PSA, age, and D'Amico risk were higher in the sELND group. Length of stay and complications were similar between the two groups. As expected, the sELND group had a higher rate of lymph node metastasis (p<.001). 13.7% of patients in the sELND group had positive nodes in the common iliac, aortic bifurcation, or pre-sacral chains. 3.1% of patients had positive nodes uniquely in these chains with negative external iliac, internal iliac, and obturator nodes. CONCLUSIONS: A subset (13.7%) of high risk prostate cancer patients have positive nodes outside of the ELND template. Patients with positive nodes uniquely in the super-extended template (3.1%) would have been under-staged had an ELND been performed. sELND for high risk prostate cancer is feasible and safe. Further studies are needed to determine clinical benefit. 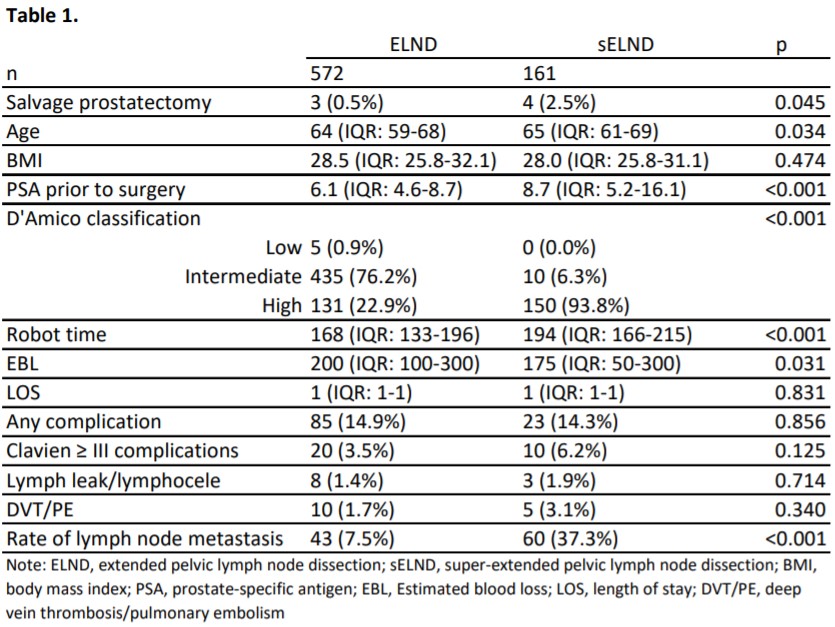
Back to 2022 Abstracts


