Feasibility of Nonlinear Microscopy Technique for Evaluating Prostatectomy Margins in Real Time
May Jean Counsilman, MD1, Utsav Bansal, MD1, Yuchen Liu, BS, BA1, Yue Sun, MD1, Seymour Rosen, MD1, Lucas Cahill, PhD2, Tadayuki Yoshitake, PhD2, James Fujimoto, PhD2, Yubo Wu, DO1, Catrina Crociani, MPH1, Allison Kleeman, BS1, Jeffrey Sun, BS1, Timothy Weber, PhD2, Sagar Doshi, BS2, Peter Chang, MD, MPH1, Andrew A. Wagner, MD1.
1Beth Israel Deaconess Medical Center, Boston, MA, USA, 2Massachusetts Institute of Technology, Cambridge, MA, USA.
BACKGROUND: Treatment of prostate cancer with radical prostatectomy can have significant side effects including urinary incontinence and erectile dysfunction. Nerve sparing radical prostatectomies (NS-RP) help reduce these effects but come with a risk of compromising oncologic outcomes. Intraoperative margin evaluation using frozen section during RP has been shown to improve nerve-sparing rates and decrease positive surgical margins (Schlomm et al 2012) but is time and resource-intensive and has not been widely adopted. Nonlinear microscopy (NLM) is a novel technology that can quickly image fresh surgical specimens at adjustable depths and produce digital images resembling standard hematoxylin and eosin (H&E) histology. We have previously demonstrated the ability to accurately differentiate prostate cancer from benign glands using NLM (Cahill et al 2020). We describe a new method to evaluate RP margins using NLM, present preliminary data on feasibility and compare NLM with paraffin embedded H&E staining.
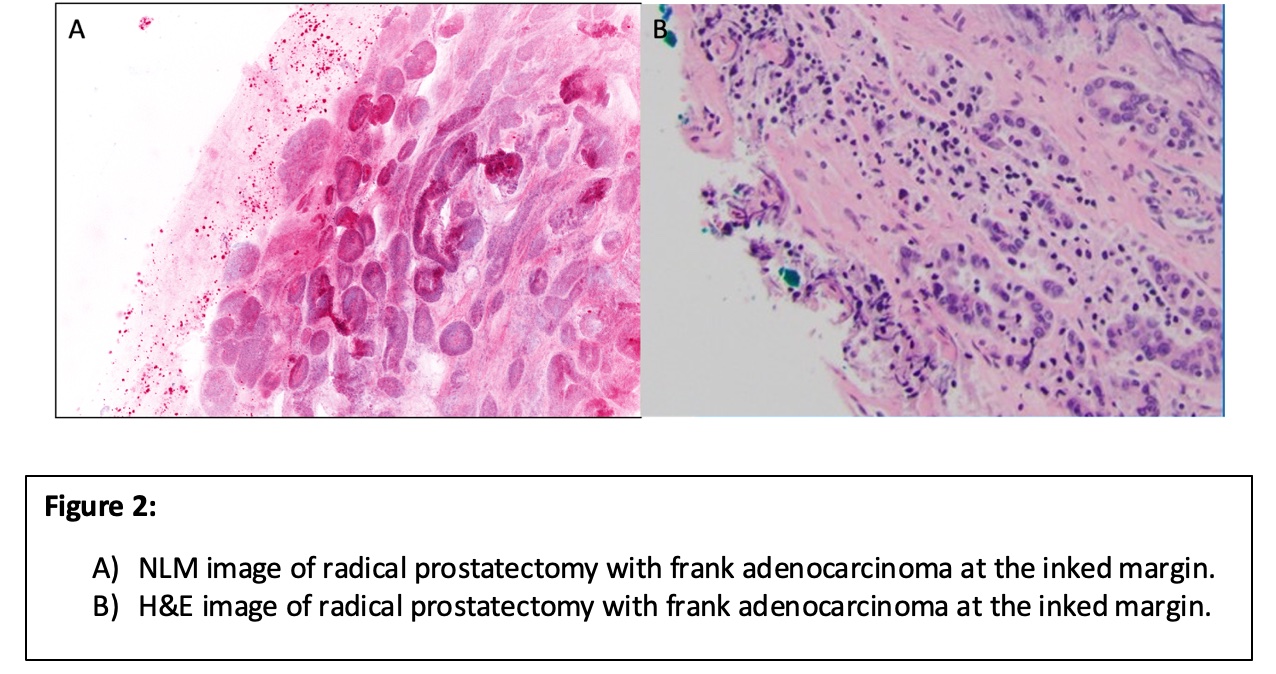
METHODS: NS-RP or non NS-RP was performed per standard of care. The specimen is inked with different tissue marking dyes combined with fluorescent plastic beads that enable the inks to be visualized under NLM. The neurovascular bundle, if present on the prostate, was dissected off ex vivo to simulate nerve-sparing and this margin inked separately. The specimen was then grossed into standard whole mount slices (Figure 1). Pathology staff were previously trained in NLM slide preparation and cancer identification. Margins were evaluated using NLM, and the tissue subsequently processed for standard paraffin embedded H&E (Figure 2). After an initial trial period of 3 patients, the timing of the NLM process was recorded to assess intraoperative feasibility.
RESULTS: 23 participants were included in the analysis. NLM evaluation correctly identified 7 cases with positive margins and 10 with negative margins. In 5 cases, tumors closely approached the margin and were cautiously deemed equivocal by NLM. All of these cases were ultimately negative on paraffin-embedded H&E. 1 case was falsely negative by NLM, but focally positive on H&E. The average time for NLM processing (inking, grossing, and evaluation) was 36 minutes. Transportation from the operating room to the NLM unit required an additional 6 minutes.
CONCLUSIONS: This study suggests the feasibility of RP margin evaluation using NLM without compromising final H&E margin status. Although not objectively analyzed, the team subjectively improved tissue handling and visualization of cellular architecture to determine margin status and we expect our times and accuracy to improve as we optimize workflow. This postoperative RP margin evaluation has helped develop a clinical roadmap for future prospective evaluation of prostate margins during RP using NLM, with the goal of increasing nerve spare RP rates and decreasing positive surgical margins without increasing operative times. 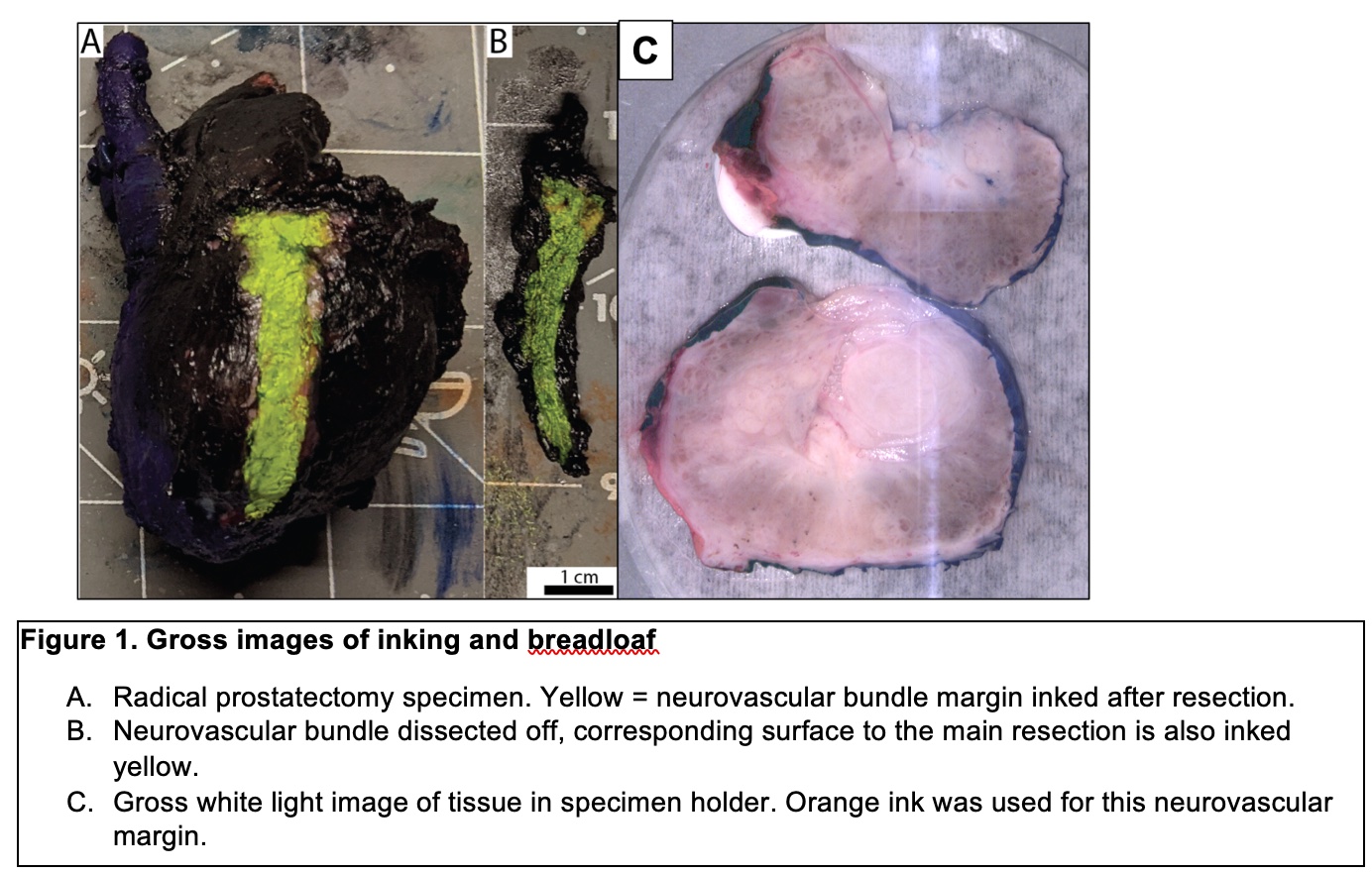
Back to 2022 Abstracts


