Radical Cystectomy Outcomes Based on Travel Distance in a Rural State
Randie E. White, MD, Joshua A. Linscott, MD, PhD, Moritz Hansen, MD, Matthew Hayn, MD, Stephen T. Ryan, MD, Jesse D. Sammon, DO.
Maine Medical Center, PORTLAND, ME, USA.
BACKGROUND:Radical Cystectomy (RC) is the standard of care for patients with non-metastatic muscle invasive bladder cancer (MIBC). Better outcomes are reported when RC is performed at high volume centers, which may lead to patients traveling further distances for care. We sought to exam the impact of travel distance on time to treatment (TTT) and clinical outcomes.
METHODS:A prospectively maintained database of 220 patients undergoing RC from 2015-2021 was retrospectively reviewed. Distance traveled to treatment center by centroid of patient zip codes was classified as <12.5 mi, 12.5-49.9 mi, and >50 mi. Complications were graded and classified by the MSKCC system. Outcomes, TTT, and readmission to outside hospital (OSH) by distance traveled were compared.
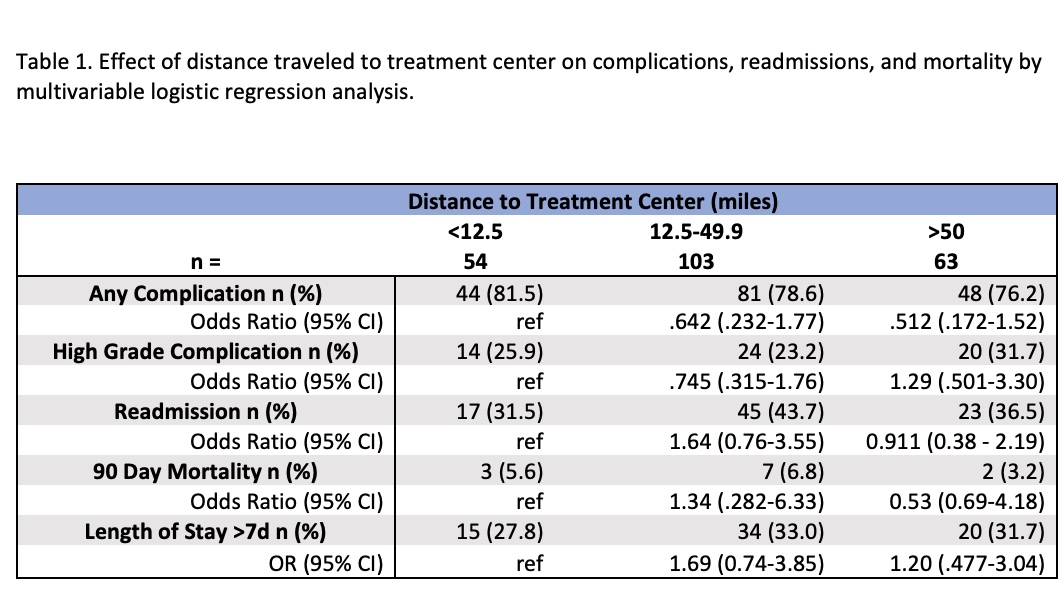
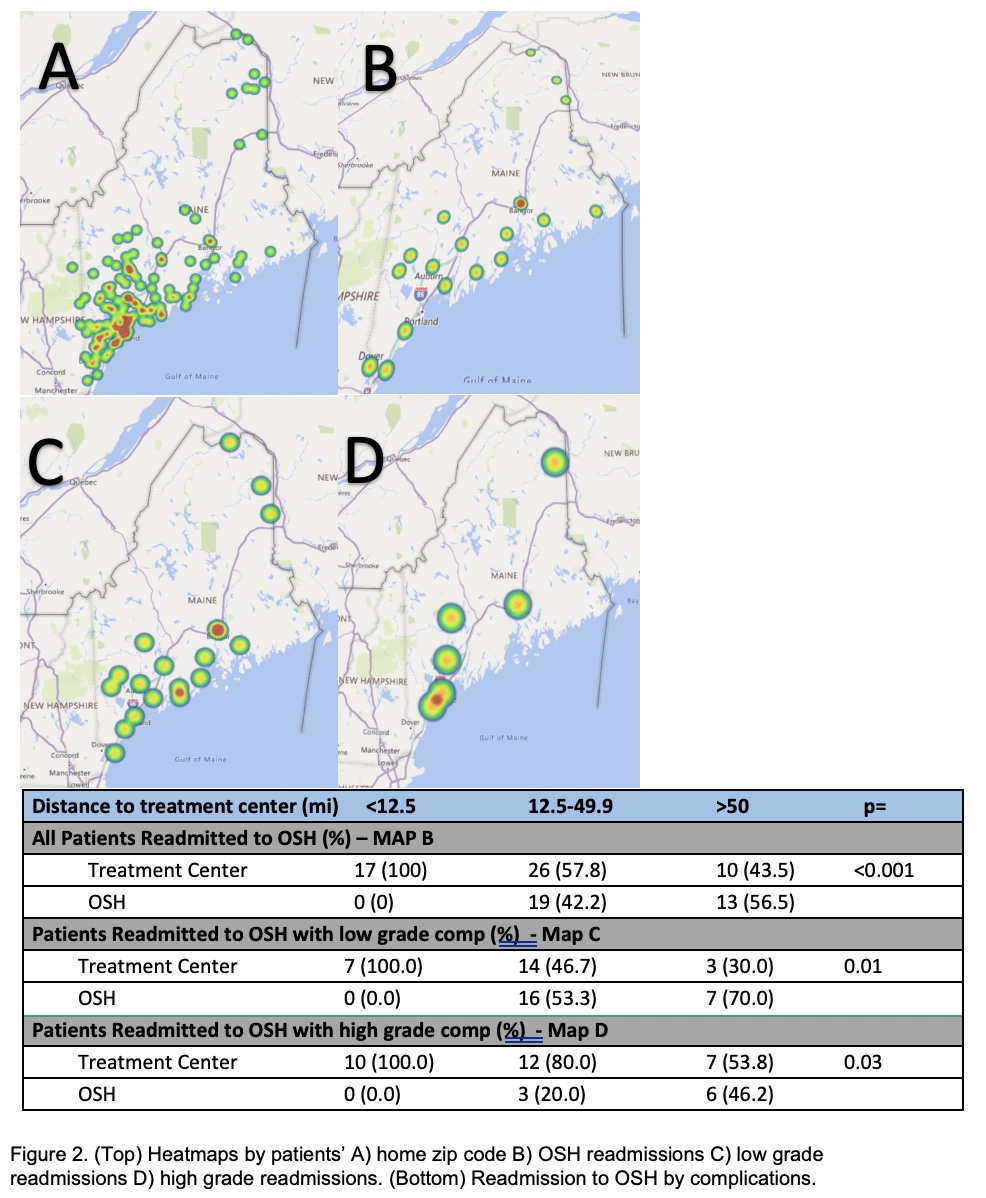
RESULTS:114 patients with MIBC received neoadjuvant chemotherapy (NAC). There was no difference in TTT with NAC (p=0.99) or time to consolidative surgery (p=0.23) by travel distance (Figure 1). For 49 MIBC patients proceeding directly to surgery, time from diagnosis to RC was increased based on distance traveled (p=0.04). There were no differences in overall complications, readmissions, 90d mortality, or length of stay (LOS) by travel distance when performing multivariable logistic regression including patient demographics and comorbidities (Table 1). All 32 patients readmitted to an OSH traveled >/= 12.5 mi (p<0.001, Figure 2). For patients readmitted with low grade complications, most traveling >12.5 mi were managed at an OSH (p = 0.01, Figure 2). The majority of high-grade complications were readmitted to the treatment center (57.8%), although OSH readmission was still more frequent if traveling >50 mi (Figure 2).CONCLUSIONS: In a rural state with one high volume RC treatment center, many patients travel long distances for care. We saw an increase in time to treatment with increasing travel distance when surgery was the primary treatment, which was not seen when NAC was the initial treatment. We attribute this to surgery being performed at one center compared with NAC available at multiple sites in a wide geographic distribution. While low grade complications may be managed close to patients' homes, high grade complications often require readmission to initial treatment center. Statewide processes and collaboration defining complications that can be treated locally versus requiring return to treatment center may help to ameliorate the challenges associated with travel distance and recovering from radical cystectomy. 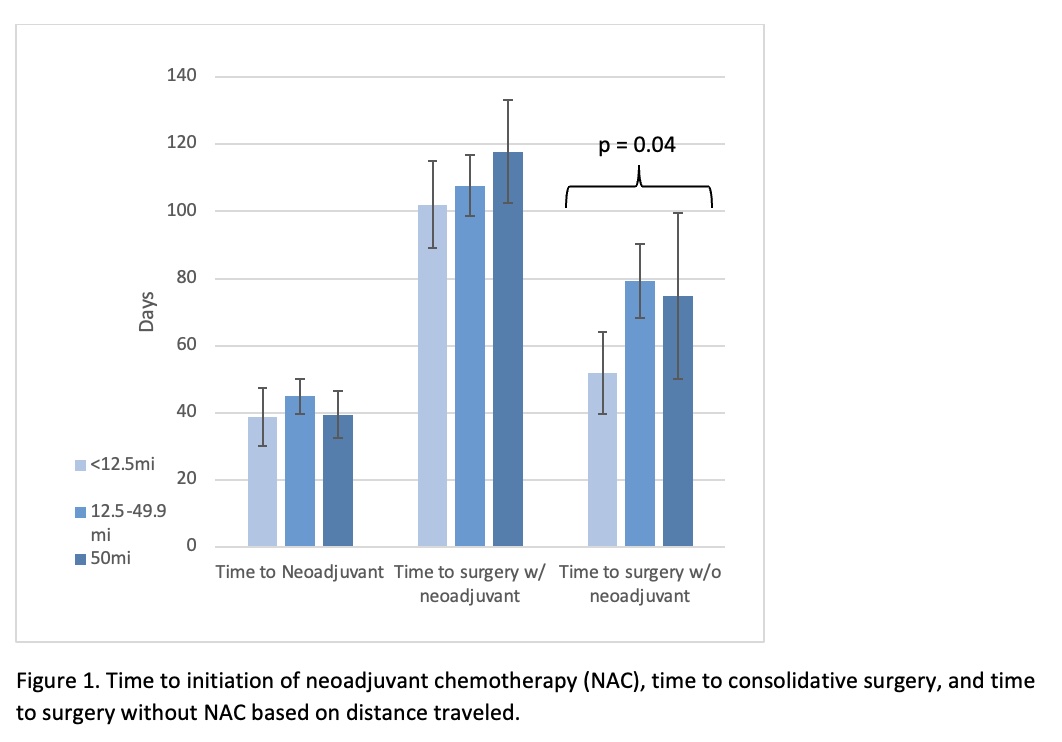
Back to 2022 Abstracts


