Baseline frailty and perioperative outcomes in older adults undergoing radical cystectomy for bladder cancer.
John Ernandez, BA1, Sumedh Kaul, MS2, Aaron Fleishman, MPH2, Ruslan Korets, MD3, Peter Chang, MD, MPH3, Andrew Wagner, MD3, Simon Kim, MD4, Joaquim Bellmunt, MD, PhD5, Nima Aghdam, MD6, Aria Olumi, MD3, Dae Kim, MD, MPH, ScD7, Boris Gershman, MD3.
1Harvard Medical School, Boston, MA, USA, 2Department of Surgery, Beth Israel Deaconess Medical Center, Boston, MA, USA, 3Division of Urologic Surgery, Beth Israel Deaconess Medical Center, Boston, MA, USA, 4Division of Urology, University of Colorado Anschutz Medical Center, Aurora, CO, USA, 5Department of Medicine, Division of Medical Oncology, Beth Israel Deaconess Medical Center, Boston, MA, USA, 6Department of Radiation Oncology, Beth Israel Deaconess Medical Center, Boston, MA, USA, 7Marcus Institute for Aging Research, Hebrew SeniorLife, Boston, MA; Division of Gerontology, Department of Medicine, Beth Israel Deaconess Medical Center, Boston, MA, USA.
BACKGROUND: The perioperative morbidity of radical cystectomy (RC) is an important consideration for optimal decision-making in older adults with bladder cancer. Frailty, a component of geriatric assessment, has been associated with the morbidity of both surgical and non-surgical interventions in this patient population. Herein, we examined the associations between a validated, claims-based frailty index (CFI) and perioperative morbidity among a contemporary cohort of older adults undergoing RC for bladder cancer.
METHODS: Using the SEER-Medicare linked database, we identified patients aged 66 to 89 years with Tany Nany cM0 urothelial carcinoma of the bladder diagnosed from 2000-2017 who underwent RC. Baseline frailty was assessed using the CFI, a validated deficit accumulation frailty measure, with a 12-month pre-diagnosis window. The associations of CFI with perioperative blood transfusion, prolonged hospitalization (defined as length of stay ≥90%-ile), and 90-day hospital readmissions were evaluated using logistic regression.
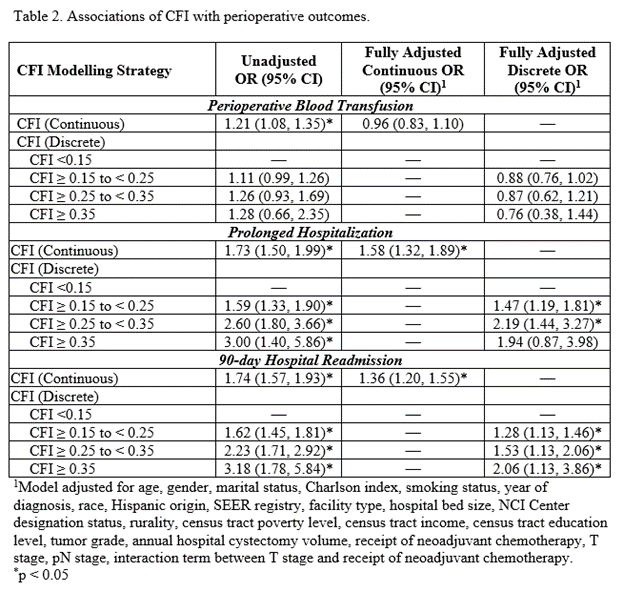
RESULTS: A total of 5,916 patients formed the study cohort, including 3,389 who were robust (CFI <0.15) and 2,527 who were pre-frail/frail (CFI ≥0.15). Overall, perioperative blood transfusion occurred in 1,499 (25%) of patients, prolonged hospitalization in 601 (10%) of patients, and 90-day readmission in 2,351 (40%) of patients. Before adjustment, increasing baseline CFI was associated with higher rates of perioperative blood transfusion, pLOS, and hospital readmission (Table 1). After multivariable adjustment, increasing level of frailty was independently associated with higher risks of prolonged hospitalization and 90-day hospital readmission, but not perioperative blood transfusion (Table 2).
CONCLUSIONS: The present study provides real-world, contemporary estimates of the perioperative morbidity of RC among older adults. Baseline frailty, as reflected by the CFI, was associated with increased risks of prolonged hospitalization and 90-day hospital readmission, even after adjusting for other patient and tumor characteristics. 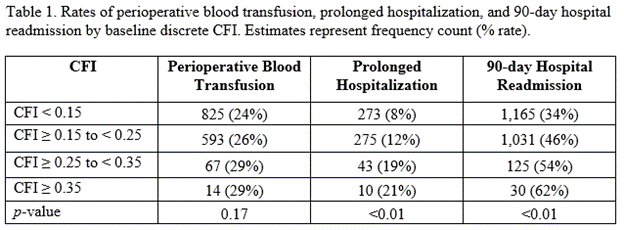
Back to 2022 Abstracts


