Urinary comprehensive genomic profiling predicts clinical recurrence in patients undergoing surveillance for urothelial carcinoma
Jason Lee, MD1, Vincent T. Bicocca, PhD2, Vincent Caruso, MS2, Brian C. Mazzarella, MD2, Kevin G. Phillips, PhD2, Trevor G. Levin, PhD2, Adam S. Feldman, MD, MPH1, Keyan Salari, MD, PhD1.
1Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA, 2Convergent Genomics, Inc., San Francisco, CA, USA.
BACKGROUND: Risk stratification of patients with urothelial carcinoma (UC) remains a major clinical challenge, with high rates of recurrence and disease progression. Urinary comprehensive genomic profiling (uCGP) has significant potential to aid in this endeavor.
METHODS: uCGP was performed on blinded urine specimens collected at Massachusetts General Hospital prior to cystoscopy. 41 subjects with a history of UC but negative by surveillance cystoscopy at time of collection were analyzed. Urine DNA was sequenced and comprehensively profiled across 60 genes using the CLIA-validated UroAmplitude test (Convergent Genomics). Patients were predicted to be at high or low risk of recurrence using a machine learning algorithm based on genomic features. Cox proportional hazards models were used to estimate the association between risk predictions and recurrence-free survival.
RESULTS: Stage and grade distribution of the primary tumor at diagnosis was Ta (73%), T1 (22%), T3 (2%), Tx (2%), with concomitant CIS in 10%; 41% low-grade (LG) and 59% high-grade (HG). Mean follow-up since specimen collection was 53.3 months. High recurrence risk was predicted in 15% (6 of 41) of subjects who had a positive UroAmplitude disease classification but negative cystoscopy. Among predicted high-risk patients, 50% had a clinical recurrence (mean time to recurrence 35.3 mo), all of which were HG. One notable high-risk patient with an initial TaLG tumor experienced a T4aHG recurrence with invasion into the prostate. uGCP-based recurrence prediction anticipated this clinical diagnosis by 17.8 months. Among 35 predicted low-risk patients, only 4 experienced recurrence (all TaLG; mean time to recurrence 20.5 mo). Recurrence-free survival was significantly worse in uGCP-predicted high-risk vs. low-risk patients (HR 4.5, 95% CI 1.01-20.2; Fig. 1). Among 10 subjects with no detectable mutations, no pathologically confirmed recurrence was observed (mean surveillance follow- up 45.3 mo).
CONCLUSIONS: uCGP can predict future recurrence of high-risk UC with substantial lead time. If validated with further studies, uCGP may provide a powerful way to risk-stratify patients and enable strategies for intensification (or deintensification) of UC management based on genomic risk. 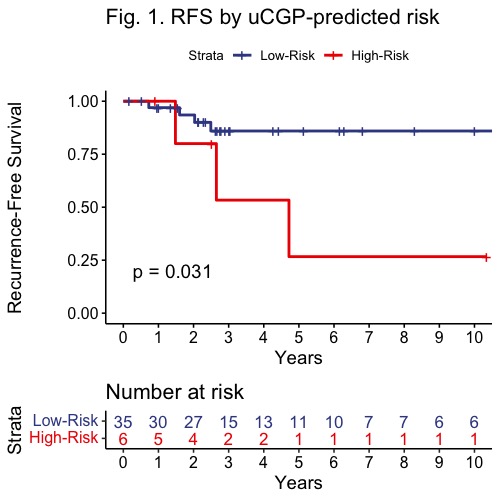
Back to 2022 Abstracts


