Comparison of MRI/Ultrasound-Fusion Trans-rectal and Trans-perineal Biopsy in the Detection of Clinically Significant Prostate Cancer: A Non-inferiority Study
Adam Wiggins, MD, William Faust, MD.
Lahey Hospital and Medical Center, Burlington, MA, USA.
BACKGROUND: Transrectal ultrasound (TRUS)/MRI-fusion biopsy has been shown to increase diagnostic yield compared to the conventional TRUS 12-core template methodology. Currently, Transperineal (TP) prostate biopsy is gaining increased clinical interest as a safe and effective approach to sample the prostate gland with less risk of infection and bleeding than TRUS biopsy. However, compared to (TRUS)/MRI fusion, the diagnostic efficacy of TP/MRI fusion biopsy—measured via cancer detection rate (CDR)—is not fully understood. Thus, this study seeks to better elucidate the effectiveness of TP/MRI fusion as a contemporary biopsy approach through comparing cancer detection rates between software-based TRUS/MRI- and TP/MRI-fusion prostate biopsy.
METHODS: MRI/US Fusion prostate biopsies performed between 2019 and 2022 using either a TRUS- with UroNav (TRUSUN) or TP- with UroNav (TPUN) approach were analyzed. Patient characteristics including demographics, PSA, prostate volume, DRE status, highest PI-RADS lesion on MRI and final biopsy pathology were collected. Overall CDR, clinically significant Cancer Detection Rate (csCDR), and clinically significant cancer detection rate in target lesion only (csCDRt) were compared between the two biopsy approaches. Statistical analysis was performed using chi-squared and t-tests as appropriate.
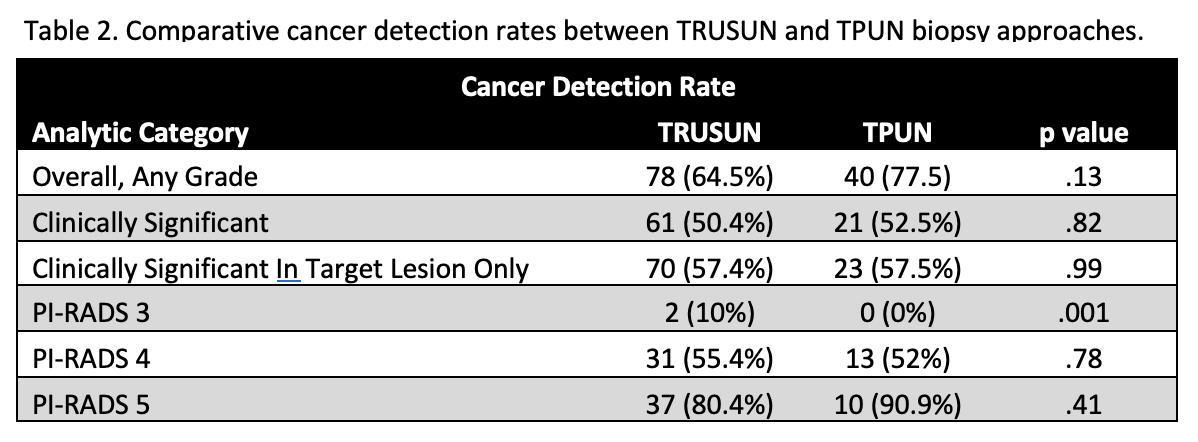
RESULTS: A total of 123 TRUSUN and 41 TPUN prostate biopsies were performed. Analysis of the total dataset showed no significant differences in baseline patient characteristics between the two groups, including age, race, smoking status, family history, diabetes, prostate volume, BMI, purpose of biopsy, PSA, and DRE findings. There were no significant differences in overall cancer detection rates between TRUSUN and TPUN approaches (p = .13). This was also the case in clinically significant cancer detection as well as clinically significant cancer detection in the target lesion only (p = .82 and .99, respectively). This remained true when stratified by Prostate Imaging-Reporting and Data System (PI-RADS) lesion designation, except for the PI-RADS 3 group, in which TRUSUN outperformed TPUN biopsy in detecting clinically significant prostate cancer (p = .001). On subgroup analysis of the PI-RADS 3 group, there were no significant differences in patient characteristics that may account for this.
CONCLUSIONS: In statistically similar patient cohorts, TPUN as compared to TRUSUN prostate biopsy showed statistically similar rates of overall CDR, csCDR and csCDRt. While a lower detection rate in those with PI-RADS 3 was noted, this is likely due to a relatively small sample size of just 5 patients with PI-RADS 3 lesions who underwent TPUN biopsy. While further data is needed to better refine these conclusions, these data suggest that the diagnostic utility gained via utilization of US/MRI-fusion in transrectal biopsy may be maintained when applied to a transperineal approach, thus bolstering the current supporting evidence for the continued adoption of TP biopsy into urologic clinical practice. 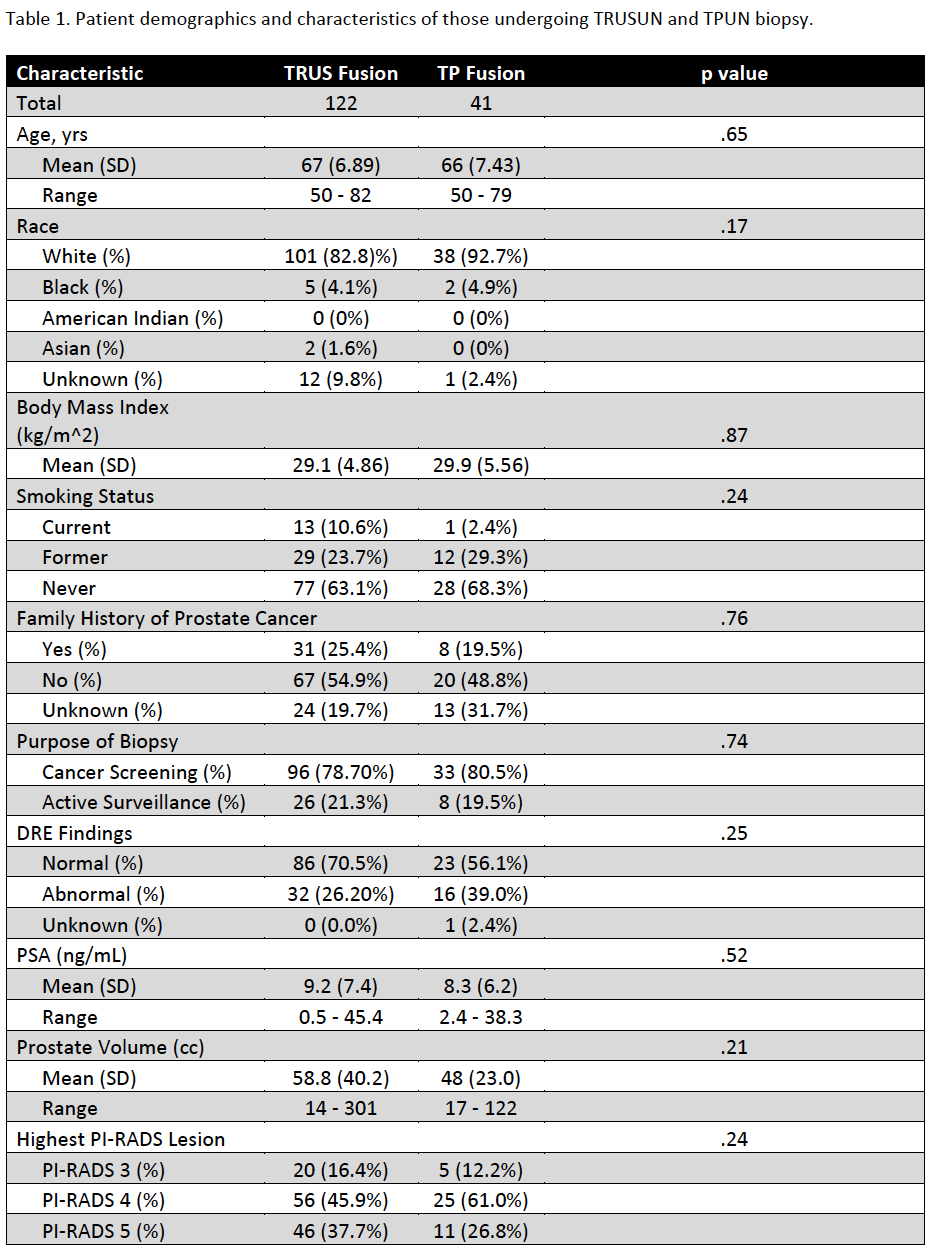
Back to 2022 Abstracts


