Lower urinary tract symptoms in patients with prostate cancer on active surveillance
Da David Jiang, MS MD1, Jeannette Schenk, PhD2, Nicholas Chakiryan, MD3, Kyle Gillis, MD4, Menghan Liu, MS2, Lisa Newcomb, PhD5, Yingye Zheng, PhD2, Peter Chang, MD1, Andrew A. Wagner, MD1.
1Beth Israel Deaconess Medical Center, Boston, MA, USA, 2Fred Hutchinson Cancer Research Center, Seattle, WA, USA, 3Moffit Cancer Center, Tampa, FL, USA, 4University of Iowa, Iowa City, IA, USA, 5University of Washington, Seattle, WA, USA.
BACKGROUND:Prostate cancer (PCa) patients on active surveillance (AS) may have concurrent lower urinary tract symptoms (LUTS) secondary to benign prostatic enlargement (BPE). Few studies have addressed LUTS in this population and guidelines are lacking on the management of LUTS for patients with PCa. The objective of this study is to describe the prevalence of LUTS and rates of bladder outlet treatment among men with PCa on AS. METHODS:Data are from the Canary Prostate Active Surveillance Study (PASS), a multicenter prospective cohort of men with PCa on AS. At enrollment and every 6 months thereafter data on medications and procedures for bladder outlet obstruction (BOO) were abstracted from medical records and assessments of LUTS via AUA symptom Score (AUASS) were completed. Men completed the enrollment and ≥ 1 post-enrollment AUASS and had a minimum of one year follow-up. Men who underwent bladder outlet procedures prior to enrollment or those with prostatitis at any follow-up visit were excluded. LUTS at enrollment were categorized as mild (AUASS 0-7), moderate (8-19) or severe (20-35). Rates of BOO treatments as well as PCa treatment were compared using univariable analyses. RESULTS:A total of 1501 men were included in the study with a median follow-up of 6.4 (IQR 3.2,9.1) years. The median AUASS at enrollment was 7 (IQR 3,11). At enrollment, the prevalence of severe LUTS was 95 (6%). Of total patients, 396 (26%) received medical treatments for BOO, 18 (1.4%) men underwent BOO procedure during the study. Compared to men with mild LUTS, men with moderate or severe LUTS were more likely to receive BOO treatments; however even among patients with severe LUTS, only 4.2% underwent bladder outlet procedures. Men with worse LUTS were more likely to have more indolent prostate cancer (Gleason Grade group 1, p=0.03); and were less likely to undergo definitive treatment for PCa (p<0.01). Among men with severe LUTS that received definitive PCa treatment, the majority underwent radical prostatectomy. CONCLUSIONS:Patients with PCa on AS with severe LUTS were more likely to harbor indolent PCa and had a low treatment rate for PCa. Although those with severe LUTS were more likely to receive bladder outlet procedures, only 4% of those patients actually did. Additional efforts are necessary to evaluate treatment paradigms for BOO in AS patients. 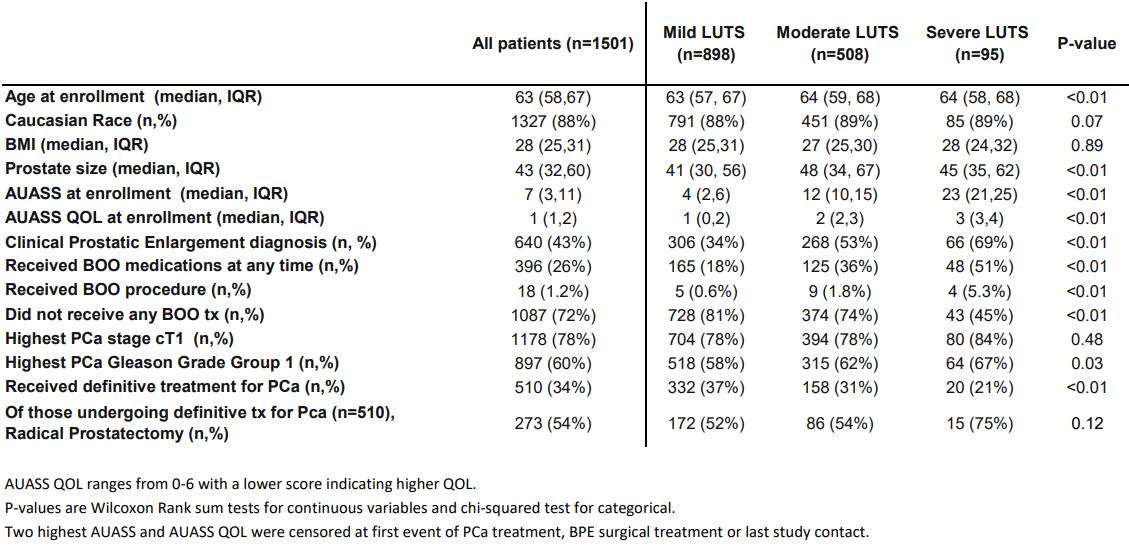
Back to 2021 Abstracts
