Lessons learned from an early Experience with Robotic Radical Nephrectomy and IVC thrombectomy
Da David Jiang, MS MD, MJ Counsilman, MD, Alejandro Abello, MD, Allison Kleeman, BS, Adrian Waisman, MD, Catrina Crociani, MS, Boris Gershman, MD, Peter Chang, MD, Andrew A. Wagner, MD.
Beth Israel Deaconess Medical Center, Boston, MA, USA.
BACKGROUND: Radical nephrectomy with inferior vena cava (IVC) thrombectomy remains a challenging and high risk surgery. This procedure is typically approached through a large chevron, thoracoabdominal, or midline incision, resulting in significant morbidity. In an effort to improve convalescence and lower complications, efforts have been made to remove the tumor thrombus and reconstruct the IVC robotically. We present our single institution experience with robotic radical nephrectomy with IVC thrombectomy as well as a video illustration of our technique. METHODS: All robotic IVC thrombectomy cases were performed by a fellowship-trained urology attending. Patients were positioned in a modified lateral position. For the left sided case, the nephrectomy portion was performed as a pure laparoscopic nephrectomy and the patient was then re-positioned for robotic IVC thrombectomy. Regional lymphadectomy was performed on all patients. The ipsilateral adrenal gland was removed in all but one patient. RESULTS: A total of 6 patients underwent robotic radical nephrectomy with level one tumor thrombectomy (into the IVC but <2cm above renal vein) between 2015 and 2021. The median follow up was 25 months (range 1-32). Patient demographics and perioperative outcomes are highlighted in the table. All patients had ECOG score of 0. Two patients had clinically enlarged regional nodes; and 2 patients presented with metastatic disease. Median operative time was 4.2 hrs (range 3.1-6.3). Median estimated blood loss (EBL) was 300mL (range 100-750) and the median hospital stay was 2.5 days (range 2-12). We performed complete IVC control using laparoscopic bulldog clamps in all patients and IVC repair was performed with either 5-0 prolene or 5-0 Gore-tex running sutures. One patient required IVC reconstruction using a bovine pericardial patch. There were no intraoperative transfusions or open conversions. The positive margin rate at the vein edge was 67%. One patient with a clinically enlarged regional lymph node had pathologically node positive disease. There was one diaphragmatic injury intraoperatively which was primarily repaired without issues. There was one postoperative 90-day complication: the first patient in our series experienced a postoperative bleed from a dislodged hemolock clip on a lumbar vein, requiring open surgical exploration 6 hours postop. Two patients had metastatic disease on presentation; they both received adjuvant systemic therapy and ultimately succumbed to their disease. Of patients who did not have metastatic disease on presentation (n=4), one patient (25%) has a recurrence in his lung and received radiation to this area, the median recurrence free survival is 12 months (range 1-38).
CONCLUSIONS:
Robotic radical nephrectomy for level one IVC thrombus in experienced hands is safe with a low incidence of perioperative complications and relatively short convalescence. 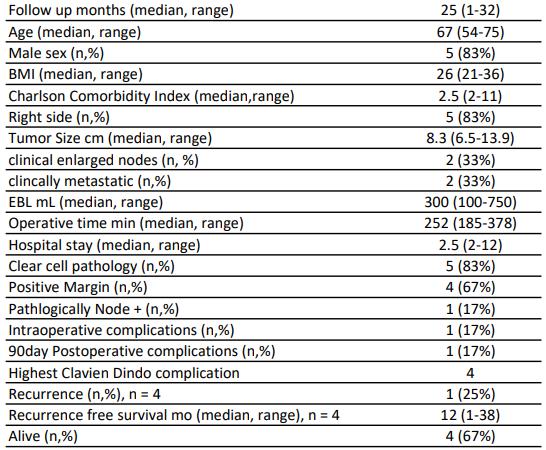
Back to 2021 Abstracts
