Demographic Factors Associated with Non-Guideline-Based Treatment of Kidney Cancer in the United States
Jeffrey M. Howard, M.D., Ph.D., Karabi Nandy, Ph.D., Solomon L. Woldu, M.D., Vitaly Margulis, M.D..
University of Texas Southwestern Medical Center, Dallas, TX, USA.
INTRODUCTION: Significant demographic disparities have been shown to exist in delivery of health care. Patients from disadvantaged socioeconomic groups are often undertreated relative to their more privileged peers in a variety of medical conditions. In patients with kidney tumors, a variety of more or less aggressive approaches may be preferred depending on clinical factors. We sought to examine the relationship of various demographic factors with receipt of both undertreatment and overtreatment in patients with kidney tumors.
MATERIALS AND METHODS: This was a retrospective analysis of the National Cancer Database (NCDB). Comparatively young and healthy patients (ages 30-70, Charlson-Deyo score 0 or 1) with localized (cT1-2 N0 M0) kidney tumors were receiving guideline-based treatment, undertreatment, or overtreatment depending on treatment choice and tumor characteristics. Relationships between demographic factors and receipt of non-guideline-based treatment were explored using univariable and multivariable regression analysis.
RESULTS: A total of 158,445 cases met study criteria, of whom 48,544 (30.6%) received non-guideline-based treatment. Results of the multivariable analysis for the overall population and clinical subgroups are summarized in Figure 1. Female sex was associated with lower risk of undertreatment (OR 0.82, 95% CI 0.77 - 0.88, p < 0.001) and higher risk of overtreatment (OR 1.27, 95% CI 1.24 - 1.30, p < 0.001) than male sex. Compared with White patients, Black and Hispanic patients were at higher adjusted risk of both undertreatment (OR 1.42, 95% CI 1.29 - 1.55, p < 0.001 for Black patients and OR 1.20, 95% CI 1.06 - 1.36, p = 0.004 for Hispanic patients) and overtreatment (OR 1.09, 95% CI 1.05 - 1.13, p < 0.001 and = 0.014 for Black patients and OR 1.06, 95% CI 1.01 - 1.11, p = 0.014 for Hispanic patients). Patterns of under- and overtreatment varied widely among clinical subgroups but were generally consistent with the overall result.
CONCLUSIONS: Significant disparities exist in treatment decision-making for kidney cancer patients, resulting in higher rates of non-guideline-based treatment for some demographic groups. Notably, this included increased risk of overtreatment as well as undertreatment for some groups. 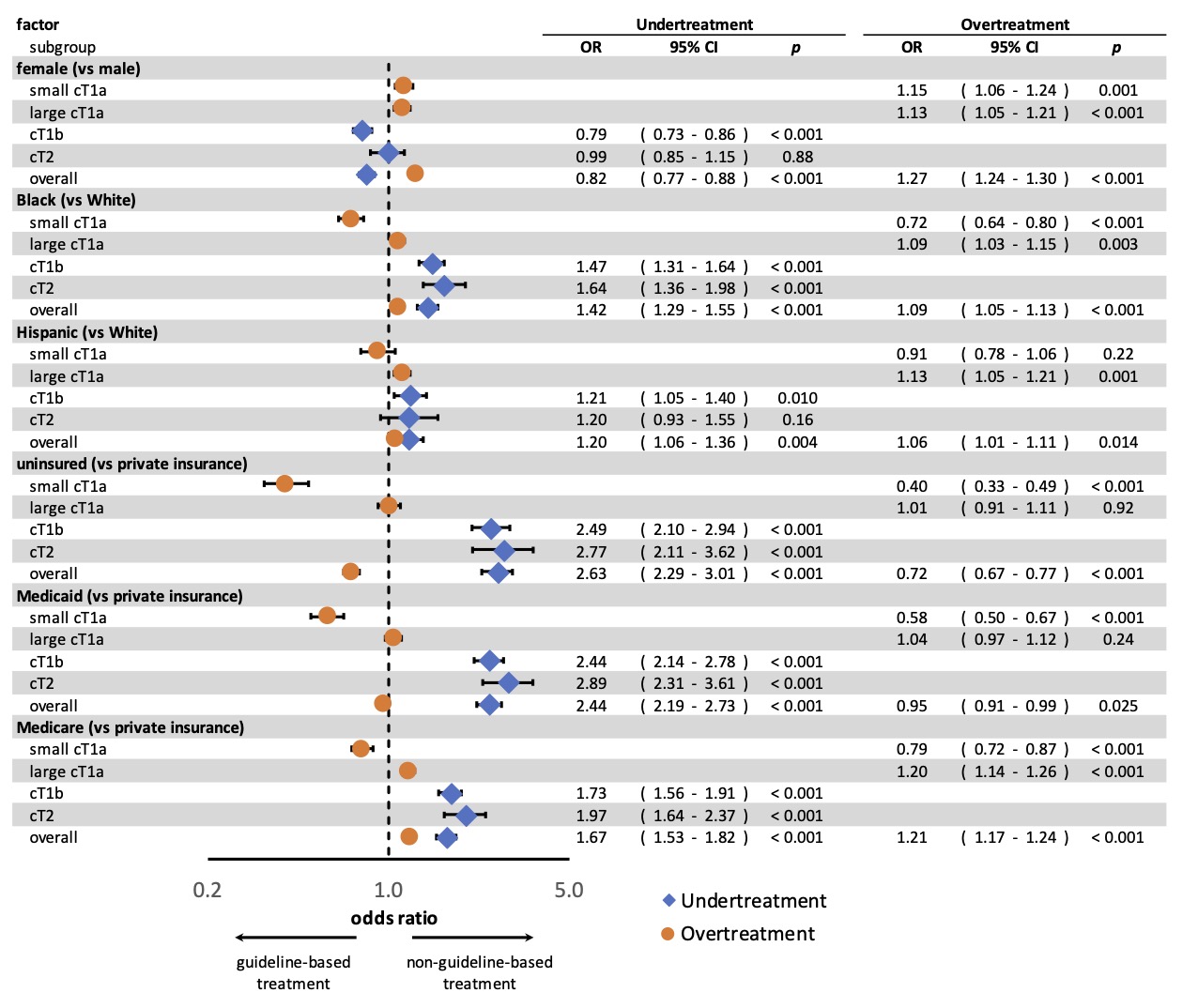
Back to 2021 Abstracts
