Presenting complaints of transgender women requiring urethral revision after feminizing genital gender-affirming surgery
Khushabu Kasabwala, MD1, Rachel A. Mann, MD2, M. Ryan Farrell, MD1, Alex J. Vanni, MD1, Nicholas Kim, MD2, Joseph J. Pariser, MD2.
1Lahey Hospital and Medical Center, Burlington, MA, USA, 2University of Minnesota, Minneapolis, MN, USA.
BACKGROUND: Vaginoplasty is the most common feminizing gender-affirming surgery performed for the male-to-female patient and is an effective treatment for gender dysphoria. More 20% of patients require re-operation for complications following surgery for functional or aesthetic issues. Voiding symptoms following surgery are distressing and non-affirming and may be related to a variety of issues including meatal stenosis or stricture, urethral angulation, urethral fistulas, or external scarring. Given the lack of standardized patient-reported outcome measures, it is often difficult to identify patients who require revision surgery for voiding-related issues. Our aim was to evaluate the presenting symptoms of patients who required revision surgery for voiding complaints after feminizing vaginoplasty.
METHODS: We performed a retrospective review of all patients who had revision surgery for voiding complaints after feminizing vaginoplasty for gender dysphoria from January 2017 to April 2021 at two institutions. Demographic and clinical characteristics, including pre-operative voiding complaints and exam findings, as well as surgical data were reviewed for each subject.
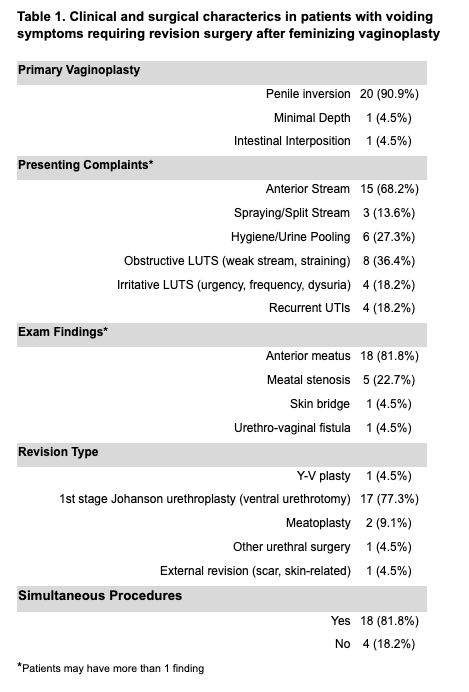
RESULTS: A total of 22 patients were identified. The median age at revision urethral surgery was 39 (interquartile range [IQR] 30-61) years. The median time from date of primary vaginoplasty to reconstructive urethral surgery was 39 (IQR 15-50) months. The majority of patients had prior penile inversion vaginoplasty (n= 20, 90.9%). Most patients presented with 2 or more voiding complaints (n = 15, 68.2%). The most common complaints included anterior stream (68.2%), weak stream and straining (36.4%) and hygiene issues including urine pooling (27.3%). Anteriorly located urethras (n=15, 68.2%) were the most common indication for subsequent urethral surgery, followed by meatal stenosis (n=5, 22.7%). Revision surgery was done in a majority of patients using a ventral urethrotomy or 1st stage Johanson urethroplasty (90.9%). At the time of urethral revision, 18 patients (81.8%) had simultaneous procedures performed (such as labiaplasty, clitoroplasty, or procedure for canal stenosis). CONCLUSIONS: PPresenting complaints for revision urethral surgery after primary vaginoplasty can be diverse and evaluation of the external genitalia is essential for diagnosis and surgical planning. The most common complaint was deviated urinary stream secondary to an anteriorly-located meatus. This was most frequently repaired with first-stage Johanson type urethroplasty. A thorough review of symptoms should be performed prior to surgery as patients may have other genital-related concerns that require intervention at the time of urethral revision.
Back to 2021 Abstracts
