Real-World Evidence for Pathological Downstaging of Muscle Invasive Bladder Cancer at Radical Cystectomy
Sina Hassan Beygi Monfared, BA1, Sumedh Kaul, MS2, Aaron Fleishman, MS2, Ruslan Korets, MD1, Peter Chang, MD1, Andrew Wagner, MD1, Simon Kim, MD3, Joaquim Bellmunt, MD, PhD4, Irving Kaplan, MD5, Aria F. Olumi, MD1, Boris Gershman, MD1.
1Division of Urologic Surgery, Beth Israel Deaconess Medical Center, Boston, MA, USA, 2Department of Surgery, Beth Israel Deaconess Medical Center, Boston, MA, USA, 3Division of Urology, University of Colorado Anschutz Medical Center, Aurora, CO, USA, 4Department of Medicine, Division of Hematology/Oncology, Beth Israel Deaconess Medical Center, Boston, MA, USA, 5Department of Radiation Oncology, Beth Israel Deaconess Medical Center, Boston, MA, USA.
BACKGROUND: Pathological downstaging of muscle invasive bladder cancer to no residual disease (pT0) at radical cystectomy (RC) is an important surrogate marker for favorable oncologic outcomes. Randomized data supports increased rates of pT0 at RC with neoadjuvant chemotherapy (NAC), but real-world evidence is lacking. We therefore examined real-world rates of pathological downstaging and evaluated patient and tumor characteristics associated with pT0 at RC using a nationwide oncology dataset.
METHODS: We identified adults with cT2-4 cN0 cM0 urothelial carcinoma of the bladder diagnosed between 2006-2016 in the National Cancer Database (NCDB) who underwent RC. Rates of pathological downstaging to pT0 and pT0 pN0 were evaluated according to baseline patient and tumor characteristics. The associations of baseline characteristics with pT0 at RC were evaluated using logistic regression.
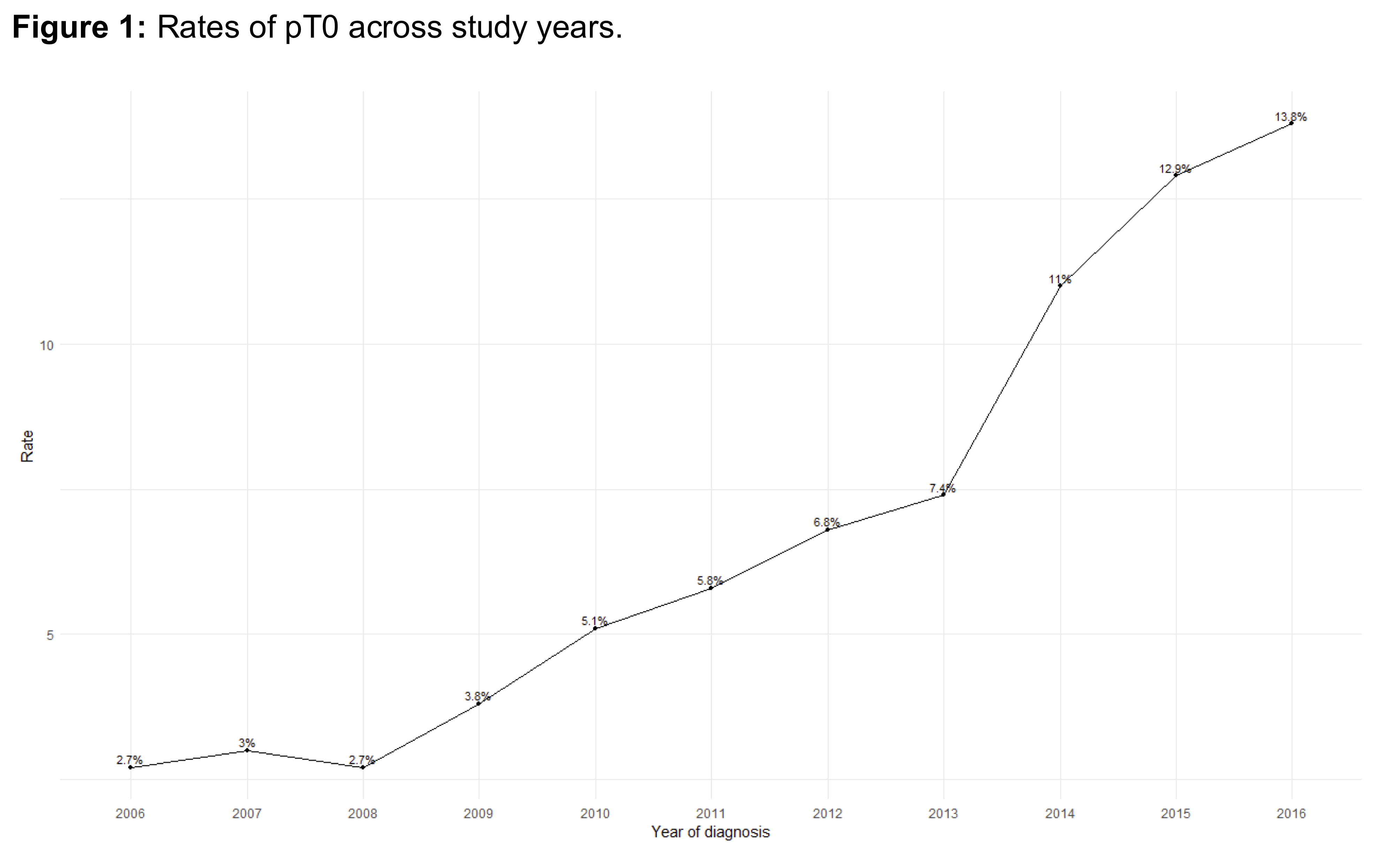
RESULTS: A total of 10,483 patients were included in the cohort. Median age at diagnosis 68 (IQR 60-75) years, and 28% of patients received NAC. The overall rates of pT0 and pT0 pN0 were 8.1% and 7.3%, respectively. The pT0 rate was 18.3% among patients receiving NAC, and 4.3% among those who did not receive NAC (p<0.01). The rate of pT0 increased across study years (p<0.01; Figure 1). On multivariable analysis (Table 1), gender (OR 0.82; 95% CI 0.69-0.98 for female vs male), later year of diagnosis (OR 3.41: 95% CI 1.91-6.75 for 2016 vs 2006), higher cT stage (OR 0.64; 95% CI 0.49-0.82 for cT3; OR 0.58; 95% CI 0.41-0.81 for cT4 vs cT1), and receipt of NAC (OR 4.14; 95% CI 3.56-4.82) were independently associated with pT0 at RC. Interestingly, higher income level and educational status were associate with increased rates of pT0 on univariable analysis but not multivariable analysis.
CONCLUSIONS: Real-world rates of pathological downstaging are lower than reported in randomized trial data. Univariable results suggest coexistent socioeconomic disparities. Of all patient and tumor characteristics examined, receipt of NAC was associated with the greatest likelihood of pT0 at RC. 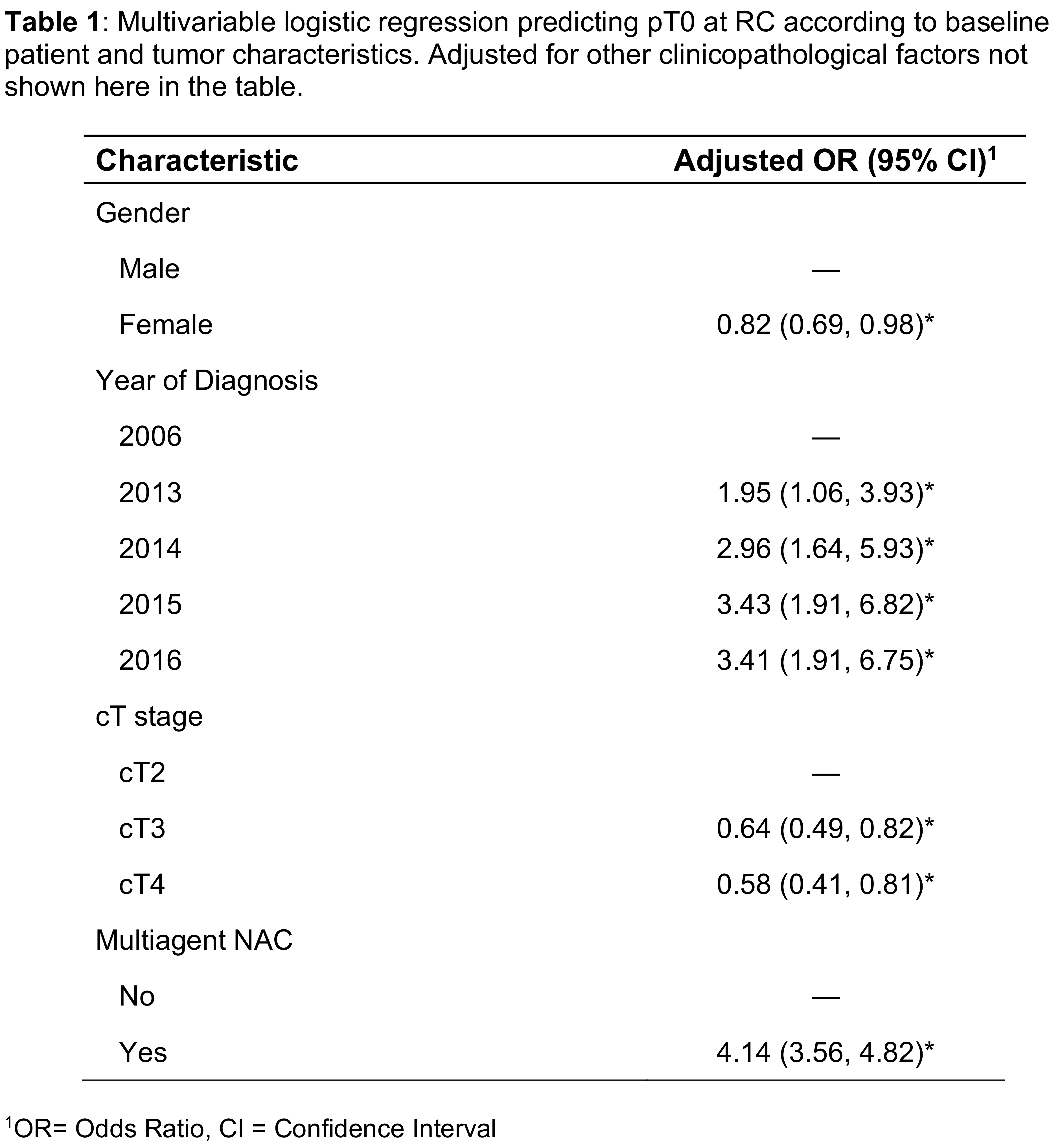
Back to 2021 Abstracts
