Radical Cystectomy with Junior Residents: Longer Days, Equivalent Outcomes
Joshua A. Linscott, MD, PhD, Randie E. White, MD, Stephen T. Ryan, MD, Moritz H. Hansen, MD, Jesse D. Sammon, DO, Matthew H. Hayn, MD.
Maine Medical Center, Portland, ME, USA.
BACKGROUND: Radical cystectomy (RC) is known to be a highly morbid, complex, and technically challenging operation. At academic centers, the assistant is traditionally a chief or senior resident. Our institution has one urology resident per year and annually performs a total of 40-50 open or robotic radical cystectomies. This leads to junior residents (PGY2, PGY3) frequently participating as the primary assistant. Here we explore the impact of resident experience level on operative, hospital, and post-operative outcomes in RC.
METHODS: A single institution, prospectively maintained database identified 159 consecutive patients who underwent open or robotic RC from 2015-2019. Residents involvement was recorded in 154 cases. Operative time, estimated blood loss (EBL), intraoperative transfusion rate, length of stay (LOS), in hospital complication, complication within 90d, readmission at 90d, and urinary diversion complications (eg uretero-ileal stricture) were compared between junior (PGY2 & PGY3) and senior (PGY4 & PGY5) residents. Patient demographics including age, sex, BMI, preoperative neoadjuvant chemotherapy, and ASA score were examined. Statistical analysis was performed with SPSS.
RESULTS: Over a 5-year period, junior residents assisted in 53 of 154 cases (34%) where a resident was involved. The number of cases done by PGY2, PGY3, PGY4, & PGY5 residents was 6, 47, 44, and 57, respectively. The percentage of open versus robotic cases was similar. There were no differences in examined patient demographics between groups. Cases with junior residents took an average of 29.1 min (CI 3.4-54.8, p=0.027) longer than when a senior resident was present. No other statistically significant differences between the two groups were seen when comparing EBL, intraoperative transfusion rate, surgical margin status, LOS, hospital complication, 90d complication, 90d readmission, or long-term urinary diversion complication (Table 1).
CONCLUSIONS: Radical cystectomy remains a challenging urologic operation demanding technical excellence. Our data suggests that participation by junior residents increases the length of operation by ~10% (29.1 min) but does not negatively impact patient outcomes. We propose this is explained by increased oversight from the attending surgeon, which allows junior residents to participate safely in an otherwise complex surgery. 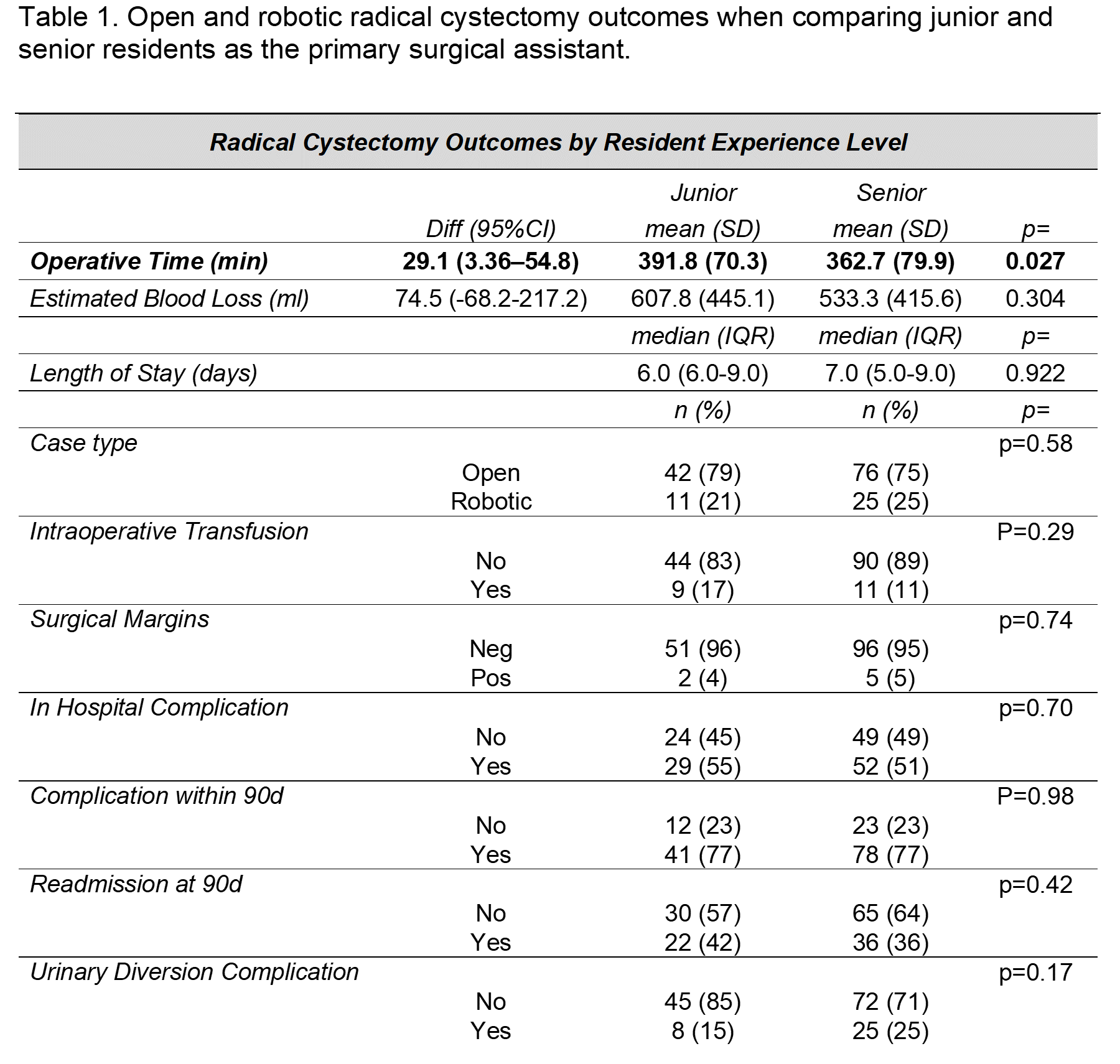
Back to 2021 Abstracts
