Radical Cystectomy in a Bubble: Catching All Complications and Readmissions
Joshua A. Linscott, MD, PhD, Randie E. White, MD, Stephen T. Ryan, MD, Moritz H. Hansen, MD, Jesse D. Sammon, DO, Matthew H. Hayn, MD.
Maine Medical Center, Portland, ME, USA.
BACKGROUND: Radical cystectomy (RC) is a highly morbid procedure with frequent complications and readmissions. Our institution is the only academic center in state and provides a vast majority of cystectomy care. A large integrated health network, EMRs, and a statewide health information exchange (HIE) make hospitalization and outpatient records readily available to us. Here we report adverse advents after RC for all patients from 2015-2019 with detailed 90d results available for every patient.
METHODS: A single institution, prospectively maintained database identified 159 consecutive patients who underwent RC from 2015-2019. Complications were graded and classified by the MSKCC system. Complications and readmissions occurring statewide for 90d after surgery were recorded and analyzed. Univariable and multivariable logistic regression analyses were conducted for all complications, high grade complications, and readmission.
RESULTS: For 159 consecutive patients, 90d follow up was available for 100% of patients and long-term follow-up was available for 101/104 (97.9%) of living patients. Patient demographics are shown in table 1. For patients with ≥cT2 disease at diagnosis 58/112 (60.7%) received neoadjuvant chemotherapy. Overall, 292 complications were recorded with 79.8%, 13.0%, and 7.2% occurring by 30d, 60d, and 90d, respectively. Individual patient highest complication grades were 0, 1, 2, 3, 4, & 5 occurring at 21.4%, 15.7%, 34.0%, 18.9%, 7.5%, and 2.5% respectively. Readmission rate was 38.4% (61/159) at a median time of 10.0 days after discharge with 22/61 (36.1%) having a diagnosis of infection related to GU source. On multivariable analysis, risk factors for any complication were Age, EBL, ASA, and intraoperative transfusion (p <0.05). No risk factors were identified for high grade complications or readmission.
CONCLUSIONS: Our types of complications (class and grade) are comparable to many large series. By incorporating outside hospital EHR, however, we noted higher than expected complication and readmission rates (78.6% & 38.4%, respectively). We believe capturing complications and readmissions statewide (up to 5 hr+ travel radius) allowed for increased detection of adverse events. This data will guide prospective studies aimed at improving patient care for a large rural state. 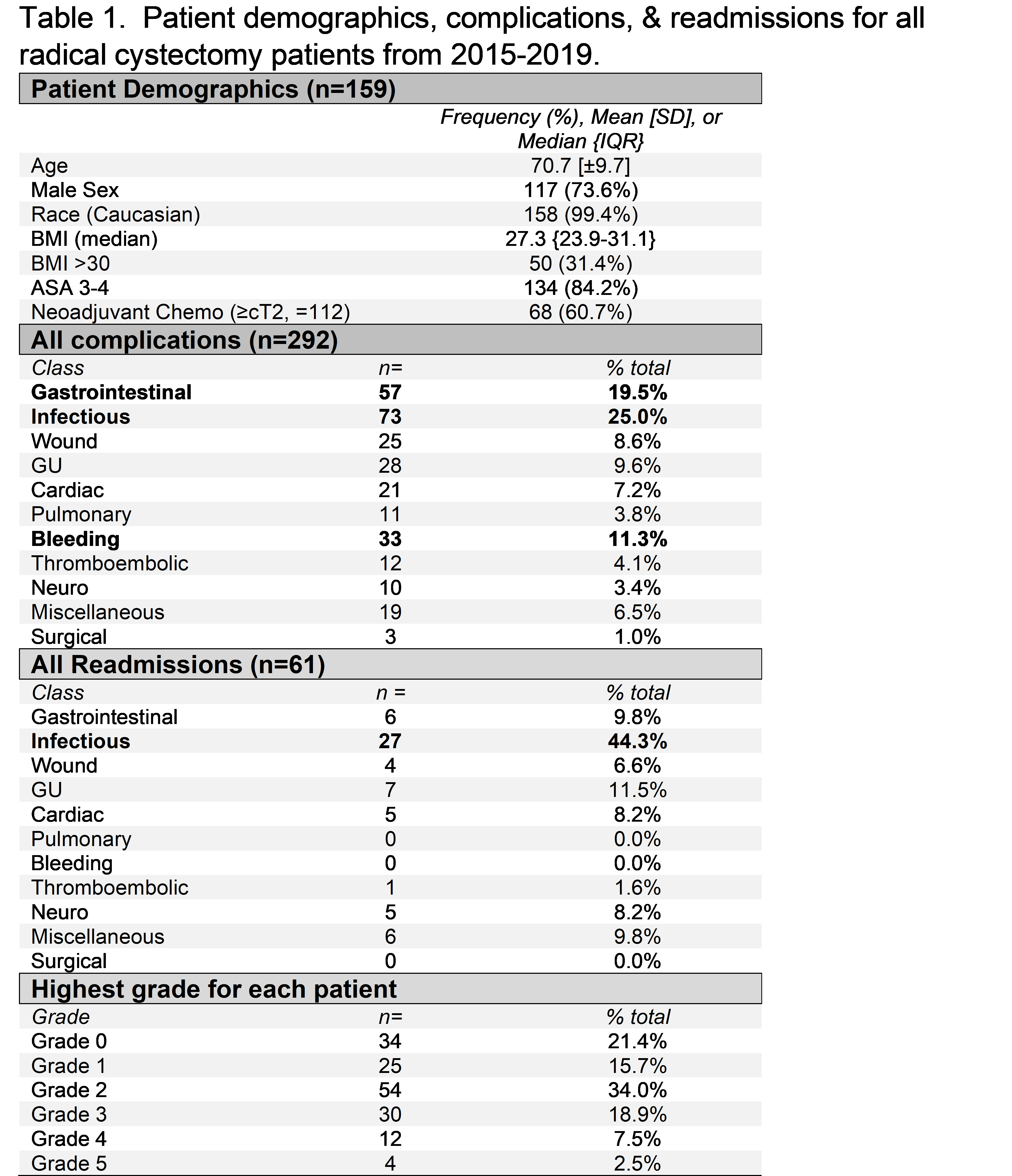
Back to 2021 Abstracts
