The "fragile" urethra as a predictor of early artificial urinary sphincter erosion
Khushabu Kasabwala, MD1, Rachel A. Mann, MD2, Jill C. Buckley, MD3, Benjamin N. Breyer, MD4, Bradley A. Erickson, MD5, Nejd F. Alsikafi, MD6, Thomas G. Smith, III, MD7, Sean P. Elliott, MD2.
1Lahey Hospital and Medical Center, Burlington, MA, USA, 2University of Minnesota, Minneapolis, MN, USA, 3University of California, San Diego, La Jolla, CA, USA, 4University of California, San Francisco, San Francisco, CA, USA, 5University of Iowa, Iowa City, IA, USA, 6Uropartners, Gurnee, IL, USA, 7MD Anderson Cancer Center, Houston, TX, USA.
BACKGROUND: Artificial urinary sphincter (AUS) cuff erosion occurs in 2-15% of patients. Some have described “fragile” urethras (previous pelvic radiation, failed AUS, or urethroplasty) to be at higher risk of erosion. Others have described risk factors such as androgen deprivation therapy (ADT), transcorporal placement, and 3.5 cm cuff. Most studies on AUS erosion have only included data on AUS cuffs placed at high volume university centers. Because university centers may have a higher concentration of high-risk men, this could skew findings through a referral bias. We sought to study risk factors for erosion among a cohort of men who underwent AUS placement by either community-based or university surgeons in order to gain a more representative sample of men and see if previously described risk factors hold true.
METHODS: This was a multi-institutional retrospective review of all patients with AUS cuff erosions who underwent AUS explant from at 6 institutions. Cuff removals were all done by university physicians, but included men who were referred for removal after AUS placement by community surgeons. Univariate analyses included t-test and chi-square test. A Cox proportional-hazards model for time to erosion was performed with the predictors being the components of a fragile urethra controlling for other previously described risk factors. Kaplan-Meier survival curves and log-rank test compared “fragile” urethras with “not fragile” urethras. All statistical analysis was done using R version 3.5.2.
RESULTS: Of the 128 men included, 38% had undergone AUS placement by community-based surgeons. Median time to AUS explant was 15.5 months (interquartile range [IQR] 5.8 - 52.2). Eighty-one men (63%) had pelvic radiation, 49 (38%) ADT, 16 (12%) prior urethroplasty, 44 (34%) prior failed AUS, 39 (30%) transcorporal cuff, and 11 (9%) had a 3.5cm cuff. One hundred men (78%) had “fragile” urethras. Radiation (Odds ratio [OR] 1.60, 95% CI 1.05-2.44) and urethroplasty (OR 2.22, 95% CI 1.23-4.00) were independently associated with earlier time to erosion. The Kaplan-Meier estimates for AUS survival time by cohort show 1- and 5-year survival rates of 71.4% and 39.3%, respectively, for “not fragile" urethras and 47.0% and 14.0% for “fragile” urethras (Figure 1, p<0.0001).
CONCLUSIONS: In a cohort of men whose AUS cuff eroded after placement by either community-based or university-based surgeons, previous findings about the “fragile” urethra held true. A “fragile” urethra remains a significant risk factor in cuff erosion; in fact, a large majority of the erosions occurred in men with fragile urethras. 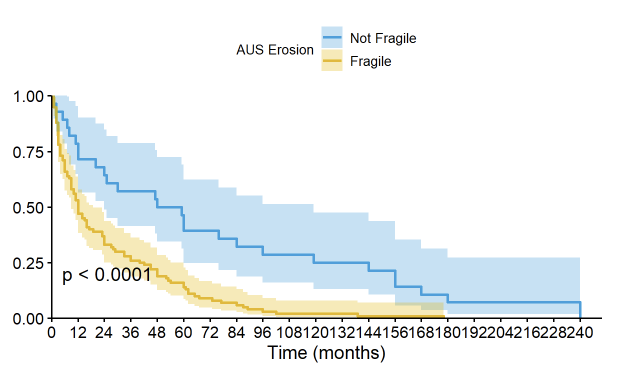
Back to 2021 Abstracts
