Association of urinary stone surgery and patient-reported complications in spinal cord injury
Khushabu Kasabwala, MD1, Michael Borofsky, MD2, John Stoffel, MD3, Blayne Welk, MD, MSc4, Jeremy B. Myers, MD5, Sara M. Lenherr, MD5, Sean P. Elliott, MD2.
1Lahey Hospital and Medical Center, Burlington, MA, USA, 2University of Minnesota, Minneapolis, MN, USA, 3University of Michigan, Ann Arbor, MI, USA, 4Western University, London, ON, Canada, 5University of Utah, Salt Lake City, UT, USA.
BACKGROUND: People with spinal cord injury (SCI) have an increased risk of urinary stone formation and an increased risk of morbidity from the surgeries to remove them. Some have postulated that the highest risk of stones is in the first year after SCI yet the natural history and health-related impact of stone disease among this patient population remains poorly defined. We hypothesized that a history of urinary stones requiring surgery would be associated with an increased incidence of SCI-related complications and lower quality of life (QOL).
METHODS: 1479 participants with SCI in the Neurogenic Bladder Research Group registry were asked about urinary stone history (pre-dating or since SCI), SCI-related complications and neurogenic bladder-related QOL. Eligibility: age ≥ 18 years with acquired SCI and followed for 12 months. Neurogenic Bladder Symptom Score (NBSS) score was used to determine bladder symptoms for QOL assessment. Continuous variables and NBSS categories were compared by the t-test and categorical variables were compared by the chi-square test (R version 3.5.2). Because the presence of stones was assessed by participant recall, we stratified our groups by history of stone surgery in order to ensure we were capturing clinically significant urinary calcifications.
RESULTS: At study entry participants were a median of 11 years post-SCI and 189 (12.8%) reported a history of bladder or kidney stones surgery; 99.5% of these occurred after the SCI. Median time between SCI and the first stone was 5.6 years (interquartile range [IQR] 1.8 - 12.8). During the year of observation, the incidence of stone surgery was 8% - 9% in those with a remote history of stone surgery and 2% per year in those without prior stone surgery (p=0.001). SCI-related complications and QOL are shown in Table 1. There was no significant difference in the rate of patient-reported UTIs but there was an increased incidence of UTI-related hospitalizations in those with prior kidney (18%) or bladder stone surgery (16%) compared to those with no stone surgery (11%, p=0.013). There was a higher rate of hospitalization for those with a history of stone surgery, with common reasons including blood clots, UTI, pressure ulcers and pneumonia (p=0.001). There was no clinically significant difference in NBSS QOL domains across the three cohorts.
CONCLUSIONS: People with SCI are at high risk for urinary stones and this risk continues over the long term. People who experience a stone are at increased risk for future stones. Kidney stones are associated with other negative outcomes such as hospitalization for UTI, pressure ulcers, deep venous thrombosis and pneumonia though they do not appear to affect QOL. People with a history of urinary stones warrant careful surveillance both for additional stone episodes and for other negative health outcomes. 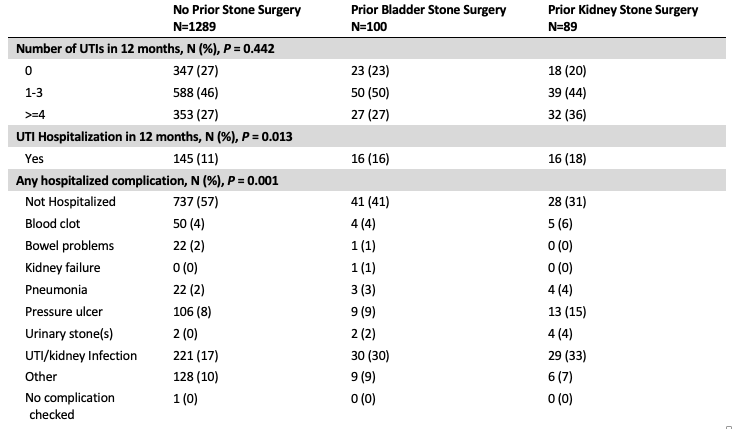
Back to 2021 Abstracts
