Computer Modeling for Optimization of Endourological Robotic Devices
Daniel C. Leslie, PhD, Liz B. Wang, MD, Max McCandless, BS, Harin Lee, BS, Sheila Russo, PhD, David S. Wang, MD, Shaun E. Wason, MD.
Boston University School of Medicine, Boston, MA, USA.
BACKGROUND: Soft robotics uses deformable materials to create minimally invasive surgical devices and has implications in endourology, where gentle manipulation of tissue is crucial. We propose a novel soft robotic anti-retropulsion device to prevent stone migration during ureteroscopy. The ideal anti-retropulsion device must be thin enough to slide past a ureteral stone, yet be able to deploy and expand to over 10mm in diameter to prevent proximal stone fragment migration. To reduce in-person laboratory work during the COVID-19 pandemic, we use commercially available software to design and test our device.
METHODS: Prototype soft robotic anti-retropulsion devices and actuators were tested in the finite element modeling (FEM) software, Abaqus (Dassault Systèmes). Material properties were programmed from previously published, experimentally validated soft robotic actuator modeling. We used Ecoflex 00-30 silicone given its superior compliance (expansion under pressure) for balloon actuation. Simulated pressure was applied to the inner surface of balloon actuators of varying dimensions, and the final geometry (deformation) after expansion under pressure was modeled.
RESULTS: Configurations of soft robotic actuators were iteratively designed and tested in Abaqus software. The initial device design was a cylindrical, 1-mm-diameter balloon tested at 0.1mm and 0.05mm thickness of Ecoflex silicone. Simulated pressure of 30kPa (4.5 PSI) and 20kPA (3 PSI) resulted in deformation diameters of 4.5mm and 7.3mm, respectively, below our ideal 10mm diameter. Final device design (below) was 1mm thick and planar, resulting in deformations greater than 12mm at 10kPa (1.5 PSI), large enough to prevent stone migration proximally in a dilated ureter. Our device conforms to the irregular geometry of the ureter upon deployment with low pressure actuation. This minimizes the potential tissue trauma when compared with current high pressure, low compliance balloons (861 kPa, 125 PSI) or metal devices.
CONCLUSIONS: Computer modeling tools enable rapid prototyping of soft robotic endourological surgical devices. We demonstrate by optimizing balloon deformation under pressure for a novel soft robotic anti-retropulsion device. Our final design can slide by ureteral stones then gently actuate over 12mm at low pressure to minimize tissue trauma. 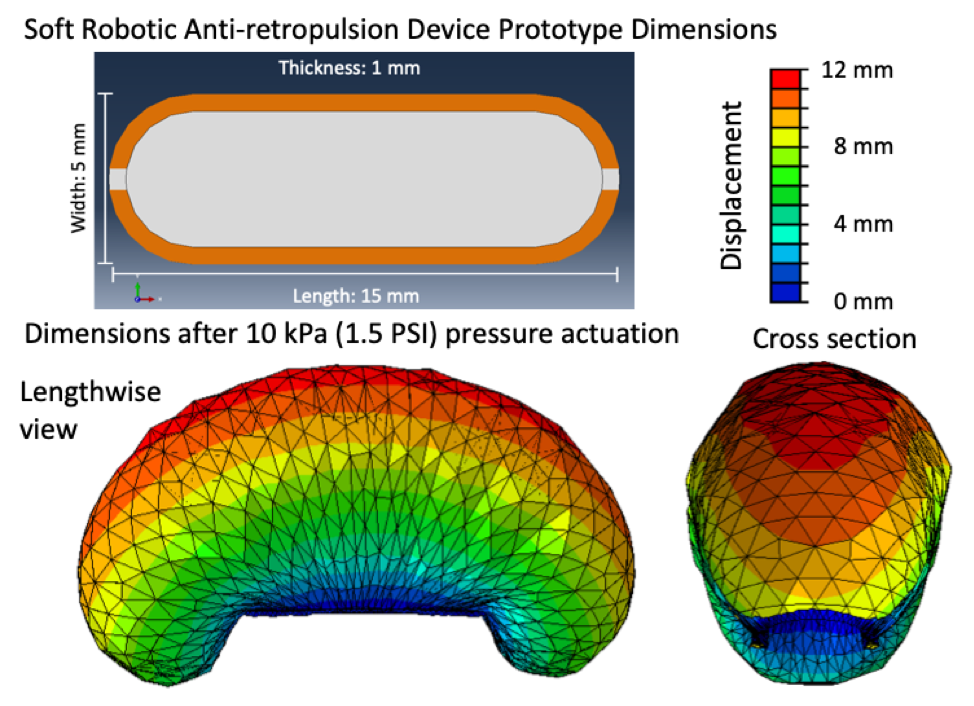
Back to 2021 Abstracts
