The COVID-19 pandemic increases opioid prescriptions following emergency department evaluation for renal colic
Siddharth Marthi, BA1, Rebecca Ortiz, BA2, Timothy O'Rourke, MD1, Christopher Tucci, MS RN1, Gyan Pareek, MD1, David W. Sobel, MD1.
1Minimally Invasive Urology Institute, The Miriam Hospital; The Warren Alpert Medical School of Brown University, Providence, RI, USA, 2Minimally Invasive Urology Institute, The Miriam Hospital, Providence, RI, USA.
BACKGROUND:
The COVID-19 pandemic has exacerbated the ongoing United States opioid epidemic; morbidity and mortality due to opioid overdose have peaked in recent months. Emergency department (ED) visits for renal colic have been sustained despite decreased visits for other nonurgenturologic complaints. Given this, we sought to quantify changes in opioid prescription patterns following evaluations for renal colic in the ED during the initial COVID-19 pandemic to evaluate whether this may have contributed to the escalating opioid epidemic.
METHODS:
A retrospective review of all presentations to an academic institution ED with primary complaint of renal colic between the initial COVID-19 pandemic in January - March 2020 as well as the same interval in 2019 (January - March) was performed. All opioid medications administered inthe ED and prescribed at discharge were included in the analysis. Using standard conversion factors, the morphine milligram equivalent (MME) was calculated for each prescription, and t-tests were performed to assess differences in total opioid dose amounts between the two time intervals.
RESULTS:
A total of 523 evaluations for renal colic in the ED were included in the analysis. 257 renal colic presentations occurred between January-March 2019 and 266 between January-March 2020. The total dose of opioids in MME prescribed on discharge was significantly higher in 2020 (Mean = 74.0, SD = 30.6) than in 2019 (Mean = 65.8, SD = 32.3; t = 2.040, p = 0.0424). Rates of prescription of over 30 MME/day on discharge in 2019 and 2020 were 4/257 (0.02%) and 15/266 (0.06%), respectively. No significant difference between these two groups was detected for opioid MME administered in the ED (t = 0.372, p = 0.710) or in the ED and at discharge combined (t = 0.485, p = 0.628).
CONCLUSIONS:
Patients who presented to the emergency department at our institution were discharged with more opioids during the initial COVID-19 pandemic than in 2019, however, they were treated with similar doses of opioids while being evaluated in the ED. Providers should be aware of these trends in prescription patterns and avoid over-prescription of opioids. Future research is warranted to better provide patients suffering from acute renal colic with adequate analgesia while minimizing possible contributions to the opioid epidemic. 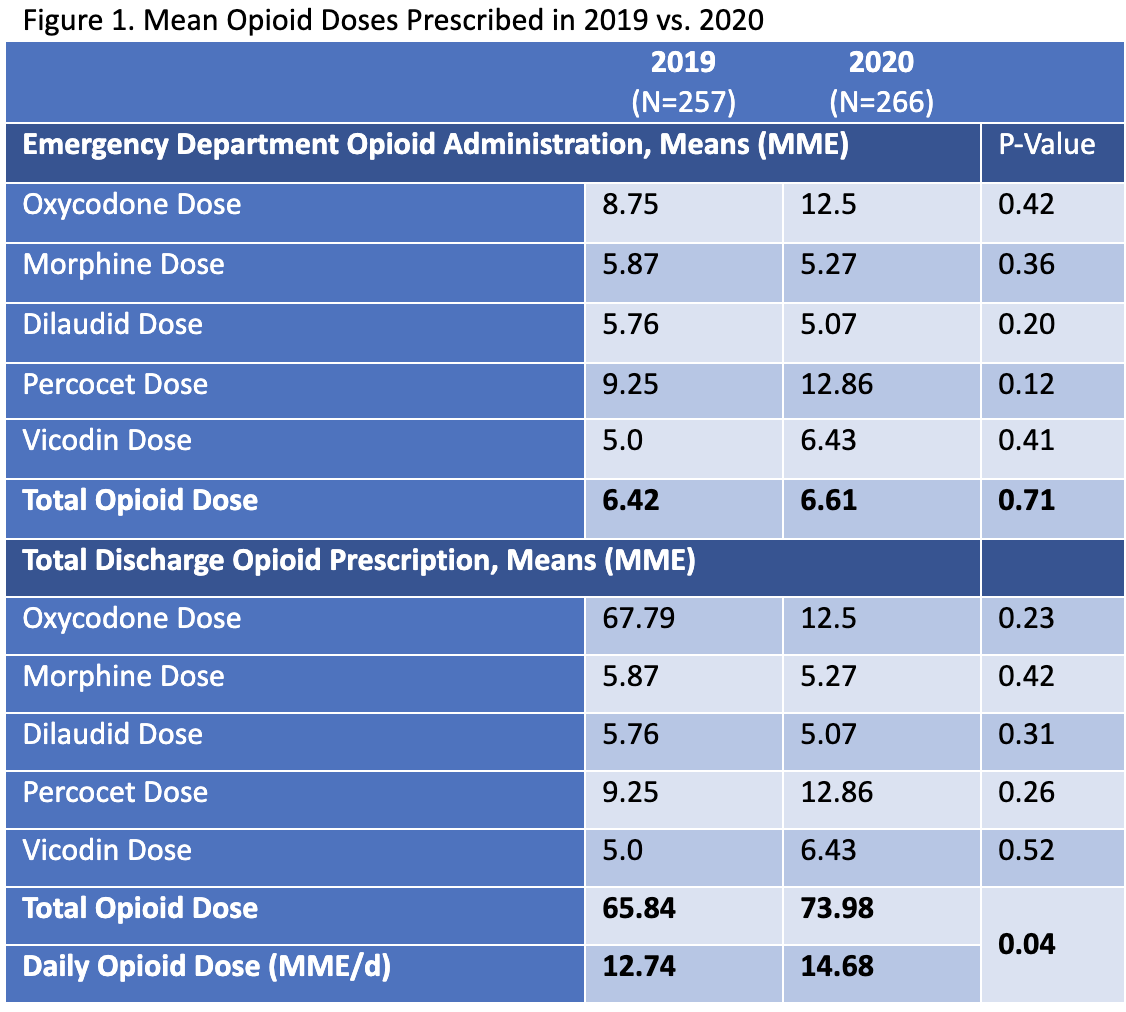
Back to 2021 Abstracts
