Testing for Racial Sampling Bias in the National Cancer Database: Does the NCDB Adequately Represent Racial Minorities with Genitourinary Cancers?
Kyle Michelson, BA1, Danielle Gordon, BS1, Tashzna Jones, BS1, Thomas Monaghan, BS1, Raymond Khargi, MD1, Matthew Smith, MD1, Fenizia Maffucci, BS1, Hyezo Kwun, BS1, Nicholas Suss, BS1, Andrew Winer, MD2
1SUNY Downstate Medical Center, Department of Urology, Brooklyn, NY, 2Kings County Hospital, Department of Urology, Brooklyn, NY
Introduction: The National Cancer Database (NCDB) has provided data for countless studies in urologic oncology. However, no study has examined whether the NCDB equally represents genitourinary cancer patients of all races. Here we seek to delineate whether racial sampling bias is present in the reporting of primary genitourinary cancers in the NCDB by comparing it to the population-based United States Cancer Statistics (USCS) registry.
METHODS: The NCDB registers cancer diagnoses at Commission of Cancer Centers, whereas the USCS covers the entire US population. The incidence of new diagnoses of primary urologic cancers stratified by race from 2004-2015 in the NCDB was compared to the same years in USCS in order to calculate a capture rate (percentage of diagnoses in USCS also represented in NCDB). Each race’s capture rate was compared to that of white patients in order to determine statistical difference. Renal and bladder cancers were further stratified by sex. A chi-square test was performed to see if capture rates varied significantly by race.
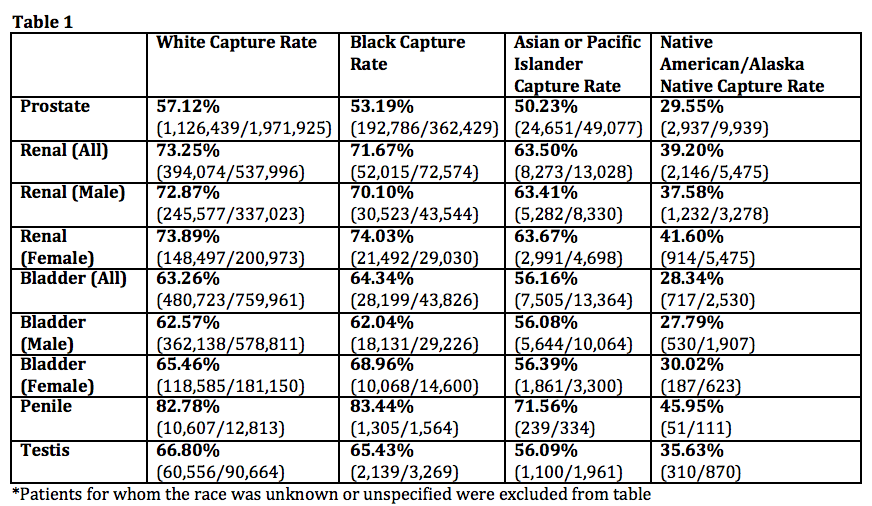
RESULTS: The NCDB captured 57.12% of the prostate cancer diagnoses for white patients found in the USCS (Table 1) versus 53.19% for black patients, 29.55% for Native American/Native Alaskan (NANA), and 50.23% for Asian or Pacific Islander (API), which are all significantly lower (p=<0.0001 for all). The capture rates for black, NANA, and API renal cancer diagnoses are each significantly lower than that of white patients (p=<0.0001 for all), with 73.25% of white vs 71.67% of black, 39.20% NANA, and 63.5% of API renal cancer diagnoses captured. This difference remained when looking at black male renal cancer patients (p=<0.0001), but not in females (p=0.5997). The capture rate was higher for black than white female patients with bladder cancer (p=<0.0001). However, all NANA and API bladder cancer patients had significantly lower capture rates than their white counterparts (28.34% and 56.16% respectively, p=<0.0001 for both). No difference was found for penile (p=0.5153) and testis cancer (p=0.1024) in black patients, but the capture rate was lower for NANA and API patients for these cancers (p=<0.0001).
CONCLUSIONS: Black male patients in the USCS with prostate and renal cancers are less likely to be represented in the NCDB than white patients, whereas female black patients with bladder cancer are overrepresented. Native American/Native Alaskan and Asian and Pacific Islander patients are universally underrepresented in the NCDB compared to white patients for all examined urologic cancers. It is vital to consider this sampling bias when interpreting NCDB-driven studies in urologic oncology.
Back to 2019 Abstracts
