Comparison of Transabdominal and Transrectal Ultrasound for Sizing of the Prostate
Wesley R. Pate, MD, Nishant Garg, BS, Liz B. Wang, MD, Shaun E. Wason, MD, Philip V. Barbosa, MD
Boston University Medical Center, Boston, MA
INTRODUCTION AND OBJECTIVES: Prostate size is an important metric utilized in the management of many urologic diseases. Imaging to estimate prostate volume includes ultrasound (US), Computed Tomography (CT), and Magnetic Resonance Imagining (MRI); however, US stands apart as a fast, radiation-free, and cost-effective modality. Two methods of ultrasound used are transabdominal pelvic (PUS) and transrectal (TRUS) ultrasound, with the latter considered to be more accurate, but more invasive. This study aims to compare the accuracy of PUS to TRUS sizing and is the largest study to date to do so.
METHODS: We performed a single-center, retrospective study of 244 patients with PUS and TRUS prostate sizing between January 1, 2012 and August 31, 2017. Prostate volume was derived from ellipsoid volume calculation using dimensions measured on US. PUS and TRUS were compared by calculating the Pearson correlation coefficient and interclass correlation coefficient (ICC), and agreement between modalities assed using the Bland Altman analysis. This analysis was done for the whole sample population as well as for specific groupings according to BMI, prostate size, and time between exams.
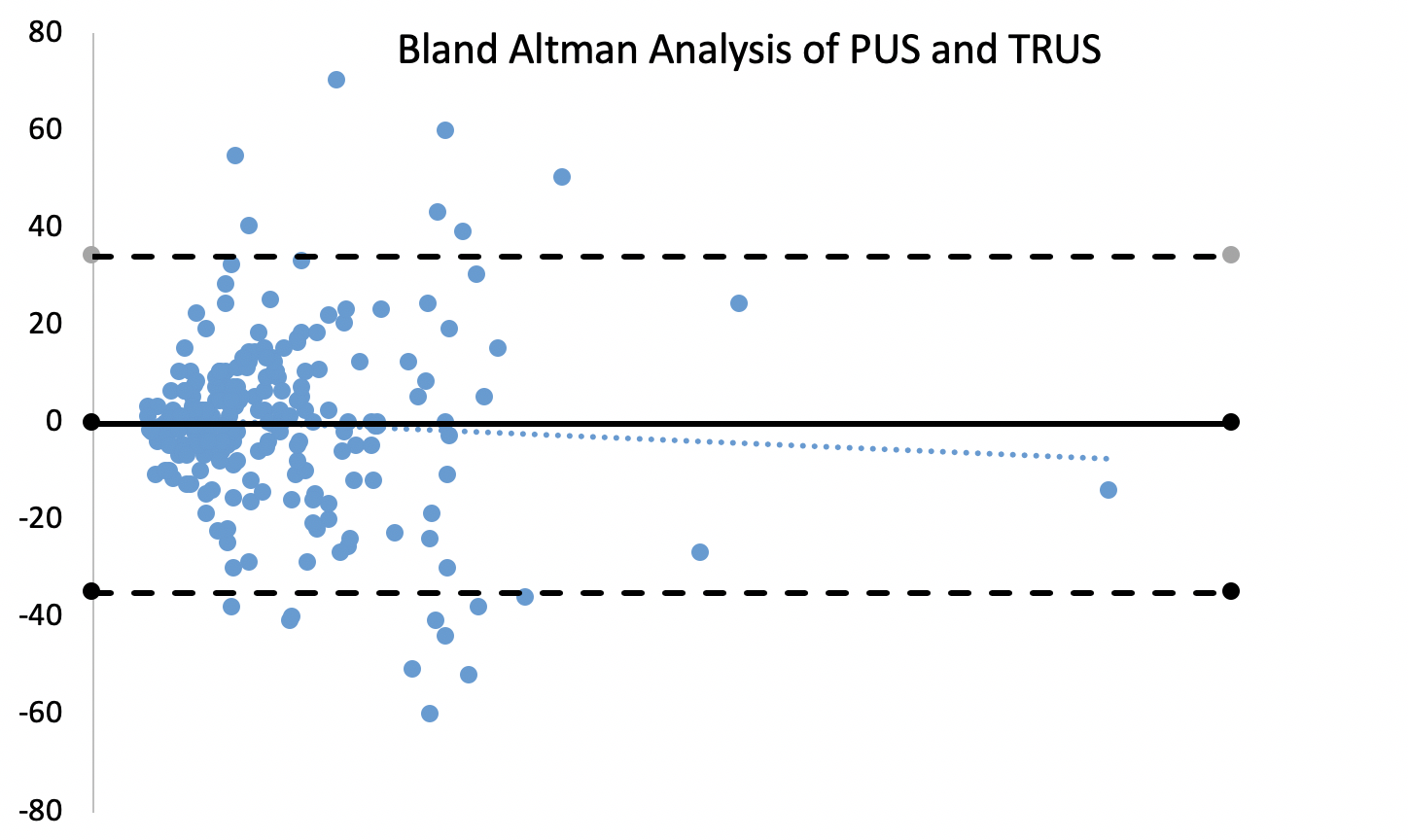
RESULTS: A total of 244 patients had both PUS and TRUS. Median age was 63 years old, median BMI was 28 kg/m2, 50 (20%) were white, 120 (49%) were black, and 41 (17%) were Hispanic. Median PSA value prior to PUS was 7.6 ng/mL. Median time between each US modality was 31 days, with 126 (52%) patients having TRUS within 31 days. The average value obtained by PUS was (63 ± 4.8) cm3 and by TRUS (64 ± 4.9) cm3. The mean of the volume differences, VolPUS - volTRUS, was (-0.2 ± 2.2) cm3, with 161 (60%) patients having a ≤ 10mL difference between PUS and TRUS estimations. Pearson correlation coefficient was 0.90, and ICC was 0.93 overall and >0.8 for all specific subgroups analyzed. Bland-Altman analysis showed 95% limits of agreement were 34/-35 cm3. When analyzed by prostate size, limits of agreement for prostates <40 cm3 and >100 cm3 are +14/-22 cm3 and +65/-58 cm3, respectively.
CONCLUSIONS: There is strong correlation between PUS and TRUS, suggesting that PUS is a useful tool for measuring prostate volume. It is important to note, however, that the Bland Altman analysis suggests that you cannot use PUS and TRUS interchangeably in all scenarios. Since PUS is non-invasive, it should be the preferred initial modality when the goal is estimating prostate size. However, if the prostate is very large or a specific volume would drastically change management decisions, one should consider utilizing additional imaging modalities. 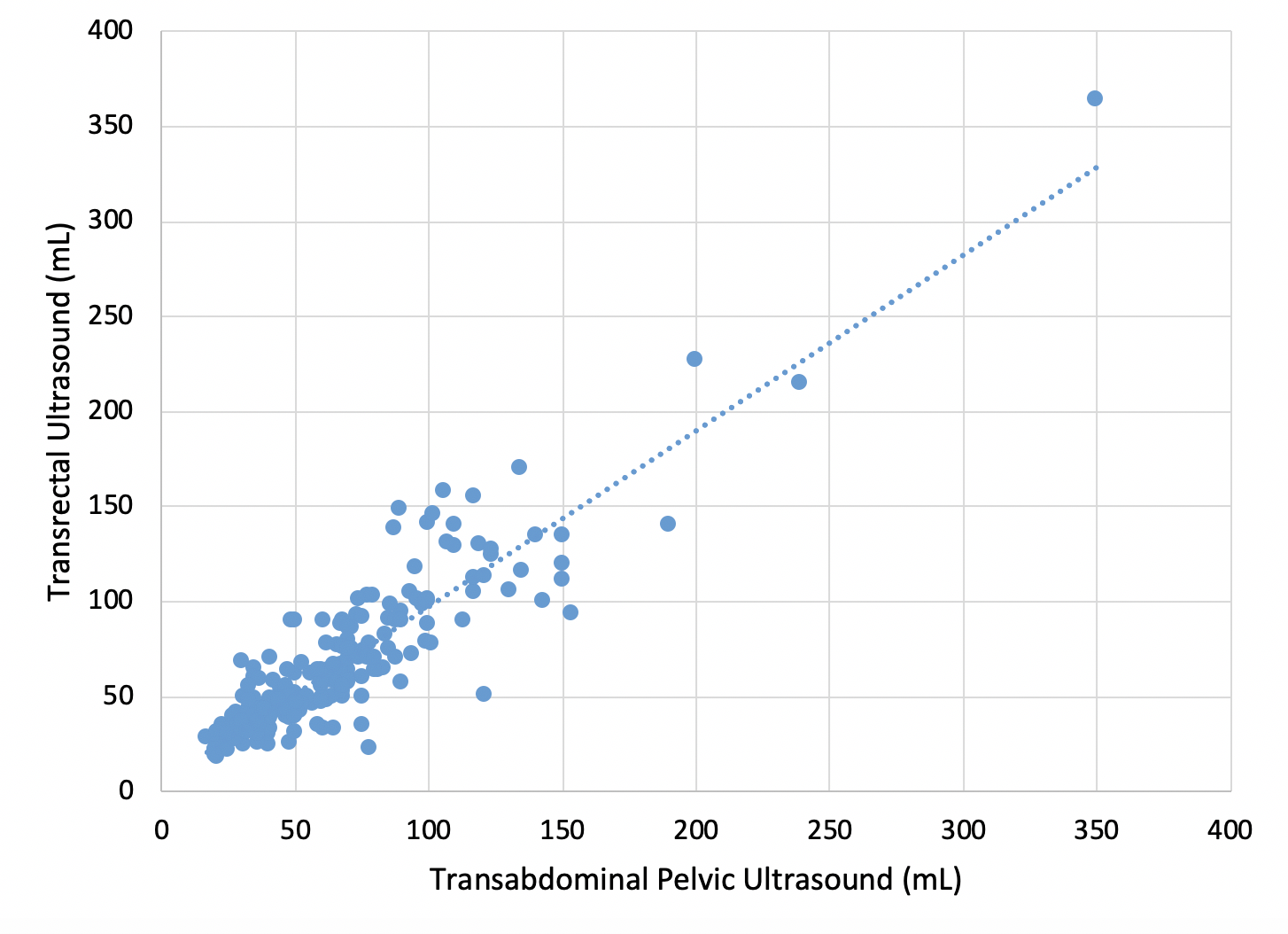
Back to 2019 Abstracts
