Economic Evaluation of Stentless vs. Stented Uncomplicated Ureteroscopy and Laser Lithotripsy
Tammer Yamany, MD, Michal Ursiny, MD, Brian H. Eisner, MD
Massachusetts General Hospital, Boston, MA
Background: Current guidelines suggest ureteral stent placement may be omitted in select patients. Complication and re-operative rates are known to be higher for stentless ureteroscopy (URS). The purpose of this study is to assess the cost-effectiveness of stentless vs stented URS laser lithotripsy using a decision analysis model. Methods: Expected value calculations with Markov modeling and sensitivity analysis were used to determine the optimal method based on overall cost-effectiveness inclusive of equipment, time, secondary costs from complications, emergency department visits, hospital readmission, and re-interventions. Data from randomized controlled trials and meta-analyses comparing stent placement and stent omission after routine URS laser lithotripsy were utilized to determine rates of emergency department visits, readmissions, re-interventions and practice patterns among urologists. Cost of operating room disposables were obtained from manufacturers. Costs of emergency department visits, readmissions, immediate and delayed re-interventions were calculated based on published figures from the literature. Costs for billable procedures were determined using published data. Results: Decision analysis modeling demonstrated that on a per-procedure basis, URS laser lithotripsy with and without ureteral stenting had average costs of $11,268 and $8,328, respectively (Figure 1). This represents an estimated savings of $2,940 per procedure without ureteral stent placement. The difference in cost for the 2 procedures was largely driven by the cost and method of ureteral stent removal. Sensitivity analysis shows that the cost difference can be minimized, but not eliminated, by increasing the rate of patient self-stent removal via string. Conclusion: Our decision analysis model demonstrates superior cost-effectiveness for URS without stent placement with an estimated savings of $2,940 per procedure. The increased costs associated with higher complication rates for stentless URS do not add increased costs to the healthcare system. Although stent omission is not recommended for every patient, careful stratification and selection of stone patients may enable surgeons to improve cost-effectiveness of URS lithotripsy. 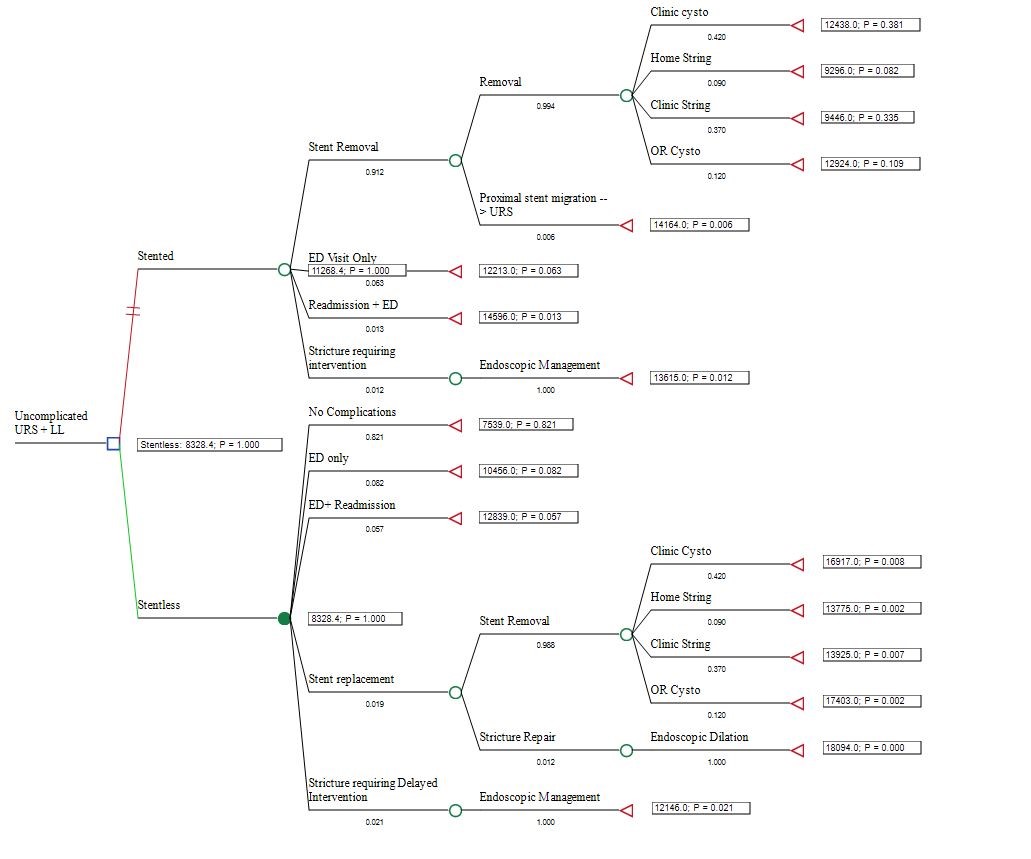
Back to 2019 Abstracts
