Recent Trends in Receipt of Palliative Care for Men with Metastatic Prostate Cancer
Alexander P. Cole, MD1, Sean Fletcher, MD2, Zara Cooper, MD1, Stuart Lipsitz, ScD1, Adam Kibel, MD1, Quoc-Dien Trinh, MD3
1Brigham & Women's Hospital, Harvard Medical School, Boston, MA, 2Harvard Medical School, Boston, MA, 3Brigham & Women's Hospital, Harvard Medical School, Brookline, MA
Background: Appropriate use of palliative care can prolong life and may reduce over-use of inappropriate end-of-life care. The past decade has seen several factors that may increase palliative care use the publication of a seminal 2010 paper showing a survival benefit for palliative care in metastatic cancer, the passage of the Affordable Care Act, and increased reporting on end-of-life care in major lay publications. We designed a study to assess trends in palliative care in metastatic prostate cancer. We hypothesized that there would be a significant rise in use of palliative care from 200462015. Methods: We abstracted data on men >40 years of age, with metastatic prostate cancer within the National Cancer Database. The receipt of palliative care is determined by trained data abstractors at participating institutions in each study year. This includes medical, surgical, or radiation therapies performed with the explicit purpose of managing symptoms but not curing disease. Routine pain control is not included. A linear spline for a multilevel logistic regression model adjusted for comorbidities, age and demographics, with a facility level random intercept was used to estimate risk-adjusted probability of receiving in palliative care in each study year. Slopes pre- and post-2010 were compared. Results: Our study cohort consisted of 52,803 men with metastatic prostate cancer diagnosed from 2006-2015. The average age was 71.3 (95% CI 71.0 - 71.5). Of these men, 5,885 (16.1%) received palliative care. On a univariate analysis, the probability of receiving palliative care in each study year increased significantly over the study period (p<0.001). However, on our risk-adjusted analysis the association between year and receipt of palliative care was only significant post-2010 (p=0.029). Advanced age and higher comorbidity score also increased the estimated probability of receiving palliative care (p<0.01 for both). The risk-adjusted probabilities in each year are summarized in Figure 1 and ranged from 11.5 (95% CI 10.5 - 12.4) in 2006 to 13.7 (95% CI 12.1 - 15.2) in 2015. Conclusions: In this study we show that the proportion of men receiving palliative care for metastatic prostate cancer gradually increased from 2006 to 2015, however the association between year and receipt of palliative care was only significant after 2010. Despite this apparently improvement only a small proportion of men with metastatic prostate cancer receive any palliative care. 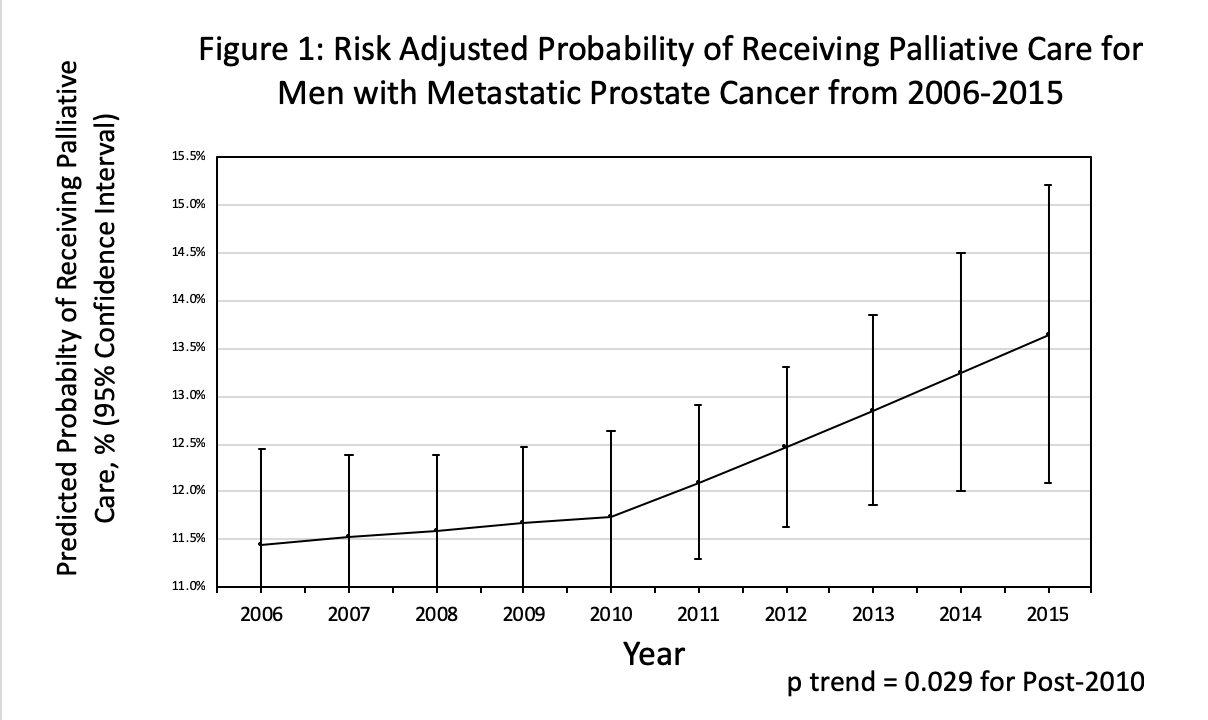
Back to 2019 Abstracts
