Characterization of U.S. Urology Resident Opioid Prescription Patterns
Gianpaolo Carpinito, BA1, Shanta Shepherd, MD2, David S. Wang, MD2, Mark H. Katz, MD2, Shaun Wason, MD2
1Boston University School of Medicine, Wellesley, MA, 2Boston University Medical Center Dept. Urology, Boston, MA
Introduction
Opioid abuse has become a national crisis. Interest in the prescription of post-operative opioids among urologists has peaked in recent years. Multiple studies have demonstrated a wide variation in the prescription of opioids by urologists. In the majority of urology practices, opioids are over-prescribed. Little is known, however, regarding opioid prescribing practices among urology residents. We sought to characterize these practices and to elucidate geographic differences in resident opioid prescriptions following common endourologic procedures.
Materials & Methods
An IRB approved, 21-question survey was distributed to urology residents at all urology programs in the US through the Society of Academic Urologists (SAU). The survey divided questions into 3 principle sections: demographic data (including AUA section), prescription patterns by endourologic procedure, and attitudes and policies surrounding opioid prescription. Endourologic procedures included ureteroscopy (URS), shockwave lithotripsy (SWL), percutaneous nephrolithotomy (PCNL) and transurethral prostate procedures (TPP).
Results
A total of 115 (9%) respondents completed the survey. On average, residents prescribed 4.7 opioid pills following SWL, 7.6 following TPP, 8.0 following URS, and 14.7 following PCNL. Using ANOVA, there were significant regional differences in resident prescription patterns following URS, PCNL, and TPP (p < .008) but not for SWL (p = .067). Those sections that prescribed the most and fewest pills on average following each procedure were identified, and significant variation from all remaining sections combined was confirmed using Welch’s t-test (all p’s < 0.006, see Table 1). Providers who believed that prescribing more narcotic pills postoperatively would decrease patient calls and ED visits were more likely to prescribe narcotics following URS (r(112) = .34, p < .001). Nationally, 79% of residents reported that their opioid prescribing patterns had decreased compared with those one year prior and 69% of residents reported working at an institution that maintains an opioid prescription policy for patients following urologic surgery.
Conclusion
Opioid prescribing practices among U.S. urology residents varied by regional AUA section and resident attitudes influenced prescription patterns. The majority of residents reported that their opioid prescribing patterns have decreased in the past year and that they work at an institution that has an opioid prescription policy. While attitudes regarding narcotics prescriptions after urologic surgery are improving, residents may benefit from additional training, best practice policies, and/or society guidelines. 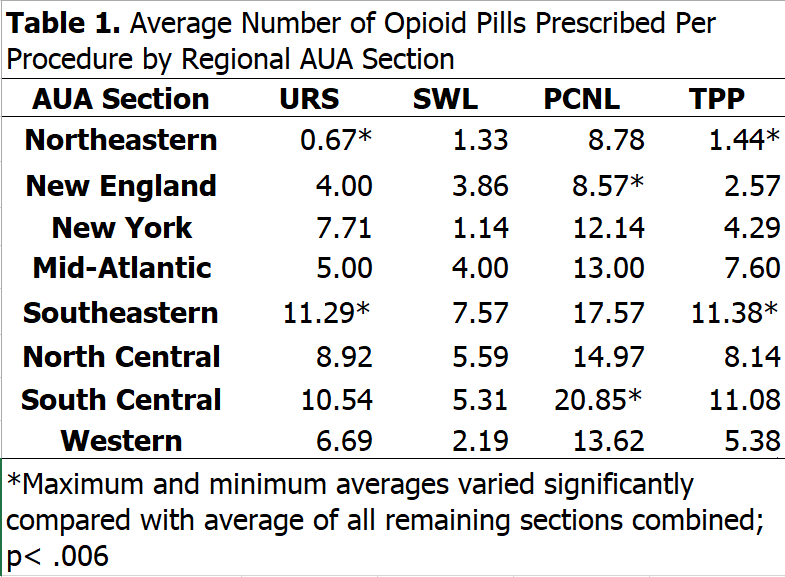
Back to 2019 Abstracts
