ProTouch Laser Enucleation of the Prostate: A retrospective analysis of the first 77 cases
Michael Emmerling, BS, Wesley Pate, MD, Shaun Wason, MD
Boston University School of Medicine, Boston, MA
BACKGROUND: The ProTouch (1470nm) laser is a novel diode laser for use in endoscopic enucleation of the prostate. ProTouch laser enucleation of the prostate (ProLEP) may provide similar outcomes to traditional HoLEP with the additional benefit of improved hemostasis and tissue vaporization.
METHODS: This is an IRB approved single surgeon chart review of 77 patients (average age 69.9 ± 9.9 years) who underwent ProLEP (10/16-3/19). Pre-operative, intra-operative, and post-operative variables were collected and analyzed.
RESULTS: Average prostate gland size was 92.4g (range: 27 - 290g) by pelvic ultrasound and average pre-operative International Prostate Symptom Score (IPSS) (on medical therapy) was 22.3 ± 6.9. Post-operative IPSS was significantly reduced at 1, 3, 6, and 12 months [12.9 ± 9.3, 9.5 ± 8.1, 7.3 ± 5.0, 9.2 ± 6.0 (p-value < 0.0001)]. Quality of life (IPSS bother scale) was significantly improved from baseline (4.7 ± 1.2) at 1, 3, 6 and 12 months [2.5 ± 1.9, 1.7 ± 1.6, 1.8 ± 1.5, 2.5 ± 1.9 (p-value < 0.0001)]. Average pre-operative Qmax was 9.1 ± 4.5 cc/sec with significant post-operative improvement at 1, 3 and 6-months [27.2 ± 11.3 cc/sec, 15.1 ± 11.1 cc/sec, 20.8 ± 6.6 cc/sec (p-value < 0.05)]. 25 patients (32.5%) were catheter dependent prior to surgery, 19 of whom had indwelling catheters while the remaining 6 performed daily clean intermittent catheterization. All patients were voiding spontaneously at 1-month post-procedure. Average operative time was 130.7 minutes and average EBL was 51.8 mL. An average of 30.4g of prostatic tissue was resected during the ProLEP procedure, with an average of 34.2% of total prostatic tissue mass resected. Thirty-eight patients (49.4%) were discharged from the recovery room, with 72 patients (93.5%) being discharged on or before POD#1. 53 patients (68.8%) had their catheters removed on or before POD#1. 14 patients (18.2%) experienced intra-operative or post-operative complications, 8 of whom required re-catheterization for post-operative acute urinary retention. Urethral false passage occurred in 1 patient, 2 patients required antibiotics for a UTI, and 1 patient underwent cystoscopy for persistent hematuria. Two patients returned to the operating room for clot evacuation and fulguration. No patients received a blood transfusion. All of the complications were Clavien-Dindo IIIb classification or less (Clavien I - 64.3%, Clavien II - 14.3%, Clavien IIIa - 7.1%, Clavien IIIb - 14.3%). No patients required repeat surgery.
CONCLUSIONS: To our knowledge, this study is the first to investigate ProLEP for the treatment of LUTS in men with BPH. Our data suggest that ProLEP is indeed a safe and effective alternative to TURP. Further studies are required to investigate the outcomes of ProLEP beyond one year. 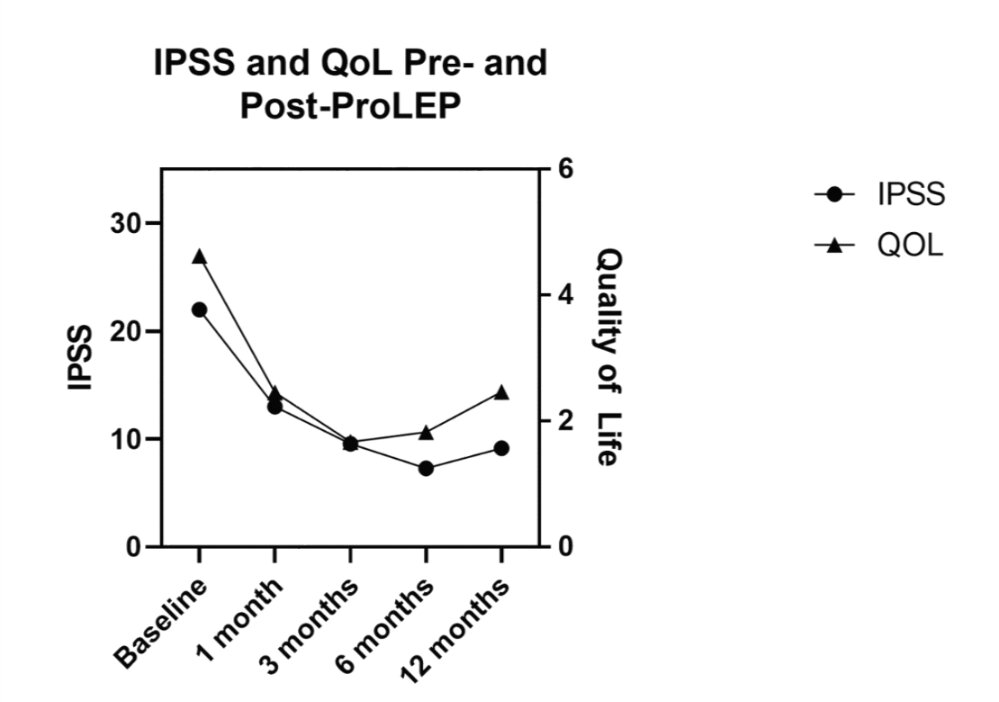
Back to 2019 Abstracts
